ANXIETY, DIABETES-RELATED DISTRESS AND THEIR ASSOCIATED FACTORS AMONG PATIENTS WITH TYPE 2 DIABETES DURING THE COVID-19 PANDEMIC
Le Thanh Nhan1, Nguyen Van Bang1,Do Thi Minh Phuong1,
Huynh Thi Bich Hoanh1, Nguyen Do Ngoc Linh1, Nguyen Van Vy Hau1,
Nguyen Thi Xuan1, Nguyen Hai Thuy2, Nguyen Dinh Toan2,
Le Van Chi2, Pham Nguyen Tuyen Linh1*
1Center of Endocrinology and Diabetes, Family Hospital, Da Nang, Vietnam
2Department of Internal Medicine, Hue University of Medicine and Pharmacy,
Hue University, Hue city, Vietnam
ABSRACT
Objective: This study aims to evaluate the prevalence of anxiety, stress and distress in T2DM outpatients during the period of the COVID-19 pandemic by using SAVE-6 and DDS-2 questionnaires to identify associated factors that affected these psychometric disorders. Method: A cross-sectional study was conducted at a medical center in South Central Coast Vietnam. 108 eligible T2DM outpatients accomplished the questionnaire utilized in this analysis. Anxiety and stress were assessed using the SAVE-6 and distress was assessed by DDS-2 scales. The sociodemographic, clinical information and behavioral changes during the pandemic were obtained through direct interviews and medical records. Identifying independent factors associated with these psychometric disorders by using multivariate logistic regression. Result: 51.9% of patients had good HbA1c control; the mean score of SAVE-6 and DDS-2 in T2DM was 8.9 ± 6.3
and 2.25 ± 1.11, respectively. According to the SAVE-6 scale, 25.9% of patients experienced anxiety and stress while approximately 63% of the participants witnessed diabetes distress based on the DDS-2 scale. Associated factors of stress and anxiety are education status (p=0.021) and hypoglycemia events (p=0.034). Education (p=0.01), abdominal obesity (p=0.01), stress and anxiety of COVID-19 (p<0.001) are related to diabetes distress. After dismissing confounding variables by multivariate logistic regressions, the result showed that low education and lack of positive behavior during the pandemic were independent factors of stress, anxiety and distress in T2DM patients (p < 0.05). Conclusion: A quarter of T2DM patients had anxiety and stress due to the COVID-19 epidemic and diabetes distress significantly increased during the viral pandemic. The information and medical supports are necessary to maintain a healthy lifestyle, positive emotions, and quality of life.
Keywords: Diabetes, anxiety, stress, distress, SAVE-6 and DDS-2
Main correspondence: Pham Nguyen Tuyen Linh1
Submission date: 19th Oct 2022
Revised date: 19th Nov 2022
Acceptance date: 19th Dec 2022
Email: [email protected]
Phone number: (+84) 793346645
- INTRODUCTION
The novel coronavirus (COVID-19) has been declared the outbreak a global pandemic by The World Health Organization (WHO) on 11th of March 2020 [5]. The virus has become a global health problem since the beginning of 2020 [17] and extended to multiple countries within a very short space of time but it is led to significantly negative effects with mass quarantine, economic loss, stressful routines, frightening morbidity and mortality [4, 16, 21, 25]. In addition, the prevalence of psychological disorders has remarkably raised at an alarming rate in the full duration of COVID-19 pandemic [7]. The lockdown, mass quarantine and the restrictions in several waves of the pandemic of community transmission are the reasons which have wreaked a negative affection on the health of the general population [9] and especially on residents who suffer from chronic diseases for example diabetes mellitus patients [13]. Diabetes mellitus (DM) is a chronic, noncommunicable disease characterized by high blood glucose levels affecting multiple aspects of human life [23]. According to the International Diabetes Federation (IDF), the prevalence of DM is 8.3%, equivalent to 463 million people worldwide [1]. IDF estimates this figure will increase to 578 million people by 2030 with type 2 diabetes mellitus (T2DM) accounting for 90% [1]. Due to the progressive nature of T2DM, patients often need more medications over time as well as nutrition therapy and routine monitoring which contributes to emotional instability and the onset of psychopathologies [2]. The lockdown and successive waves of restrictions with social distancing experiences, even though moving to isolation have disrupted healthy daily routine and the ability to self-care, intermittent balanced diet and physical regimens [14, 16]. Some studies showed that more than half of chronic patients claim to have difficulty associated to maintain their usual treatment [18] and figure from a study conducted in 155 nations by the WHO reported that there were 49% of diabetes treatment was partially or completely interrupted during the COVID-19 pandemic [6].
Diabetes mellitus patients are a vulnerable subject [31], with substantially higher hospitalization as well as mortality proportion, and this risk rises with server outcomes when they had COVID-19 infection [22]. Many studies demonstrated the marked severity and mortality of COVID-19 in DM patients from 3.9- 7.8% [26] [31] [12] [3] or mortality rates after hospitalization was increased by 66.7% with T1DM (type 1 diabetes) and by 48.5% among patients hospitalized with T2DM (type 2 diabetes) [20].
On the other side, the associated mass media coverage of the COVID-19 outbreak increased the prevalence of psychological disorders, including stress, anxiety and distress among residents in affected regions. Before the COVID-19 pandemic, previous studies showed that psychological disorders in diabetics correspond to twice the prevalence in non- diabetics [19]. These comorbidities in diabetes patients may lead to reduce self-aid, adherence to treatment and connection with health professionals, with a negative impact on disease management [8, 18].
Thus, we conducted this study to evaluate the proportion of anxiety and distress in T2DM patients and analyze the associated factors during the period of social distancing during the COVID-19 pandemic.
2. METHODOLOGY Patients and Study Design
A cross-sectional study was conducted between 1 October 2021 and 31 December 2021 at the Center of Endocrinology and Diabetes, Family Hospital, Da Nang, Viet Nam. The participants were invited to enroll in this study via a paper- survey form if they satisfied the following inclusion criteria: 1) Diagnosed with T2DM according to American Diabetes Association guidelines 2022 before the COVID-19 pandemic 2) have not had neurocognitive disorders 3) can answer the questionnaire 4) Agreed to participate voluntarily.
The sample size was calculated using the proportion with specified absolute precision, with a confidence interval of 0.95, a relative precision of 0.05 and the expected figures of anxiety among patients in COVID- 19 pandemic at 50% so the size of the sample with 97 patients would be required. However, the final sample size was increased to 108 predicting eventual losses.
Data Collection
The study was performed face-to-face via a paper- survey by well-trained staff in Family Hospital. Sociodemographic and clinical information was recorded by using a structured questionnaire to interview patients and an electronic medical records system. The participants could defer at any time from the research and not affect their current treatment. The patients’ information was kept confidential and used for research purposes only.
This instrument included questions related to the objectives of the survey: anthropometric index, sociodemographic, clinical characteristics, routine changing and psychometric disorders through SAVE-6 and DDS-2 scale during the COVID-19 period. The SAVE-6 is a self-report rating scale, which was derived from the SAVE-9 scale to measure the anxiety reaction to the COVID-19 epidemic with Cronbach’s alpha coefficient of 0.815 [29]. The DDS-2 consists of 2 items which was a brief of the DDS-17 scale for screening distress in diabetes patients. The sensitivity and specificity were 0.97 and 0.86, respectively [30].
Variable definition
Stress and anxiety due to the viral epidemic
A qualitative variable, each of the six items is rated on a five-point Likert scale between 0 (never) and 4 (always). The total score on the SAVE-6 scale ranges from 0 to 24, with higher scores reflecting higher levels of anxiety reaction to the viral epidemic. The cut-off score has been reported to be 15.
Diabetes distress
A qualitative variable confirmed by the DDS-2 scale with a mean score of <2, was considered as “no distress”; a mean score ranging from 2 to 2.9, was marked as “moderate distress”; and a mean score ≥3, was considered as “high dis- tress”
Level of changing routines
Each dimension was assessed as 0 or 1 point based on the level of changing routines of DM type 2 patients during the COVID-19 pandemic. The total score was calculated by the score of 7 items and ranged from 0 to 7, with higher scores reflecting higher levels of change in a positive trend.
Data Analysis
The statistical analysis was operated by SPSS software version 20.0 for Windows. Chi- squared test, Fisher’s exact test was applied to test the association of categorical variables; Independent T-test, ANOVA (or Mann- Whitney U test and Kruskal – Wallis test) was used to determine the difference of numerical variables in two groups: having anxiety, distress, stress groups and no anxiety, distress, stress groups. Multivariate logistic regression was performed to identify the risk factors associated with psychometric disorders in patients.
3. RESULTS
Participant characteristics
A total of 108 patients with T2DM who met the inclusion criteria were included in the final analysis.
Table 1 illustrates the demographic characteristics of participants in this study. The mean age of 59.5 ± 9.8 years was identified to characterize the sample those under 65 years old accounted for 70.4% and the mean duration of diabetes was 6.7 ± 5 years. The sample included 56.5% females. More than half were retired or elderly. 80.6% had a secondary school education or above and most of the patients reported living with family or a partner (98.1%).
Table 1. Demographic characteristics of T2DM participants in this study
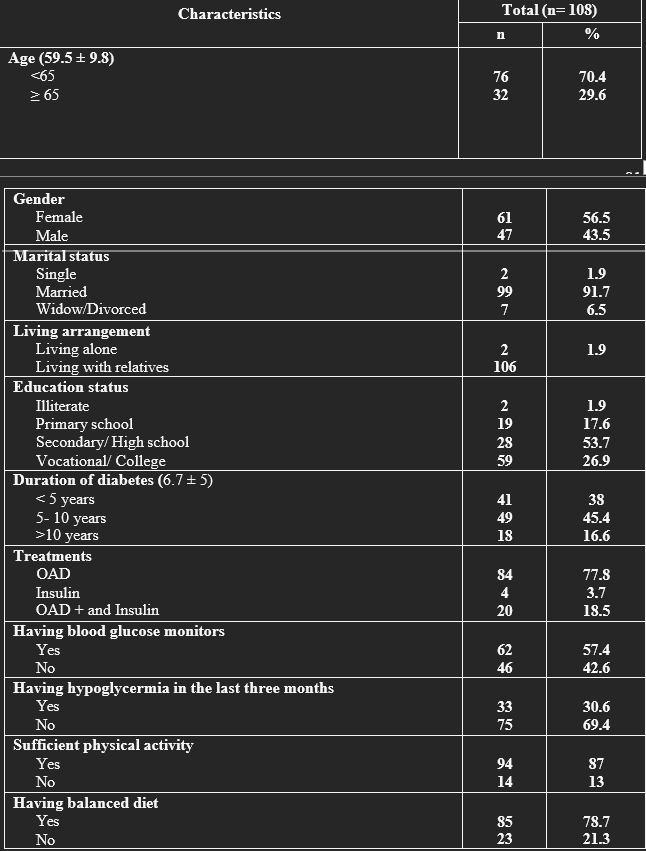
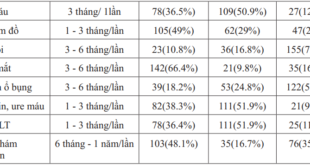
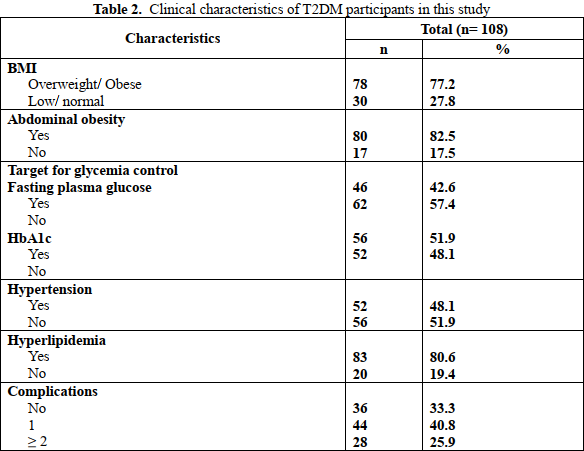
Table 2 demonstrates the clinical characteristics of T2DM participants in this study. The majority of patients were overweight or obese (78.7%). Many suffered from hyperlipidemia (80.6%) or hypertension (48.1%). 66.7% of patients had one or more complications, 77.8% were being treated with an oral antidiabetes drug (OAD), 57.9% had a blood glucose monitor at home, and 30.3% had the symptoms of hypoglycemia during three months prior to the surveyed time. As for nonmedication therapy, 87% and 78.7% of patients indicated that they consumed a complied balanced diet and had sufficient physical activity while the proportion of patients who got target fasting plasma glucose and HbA1c were 42.6% and 51.9%, respectively
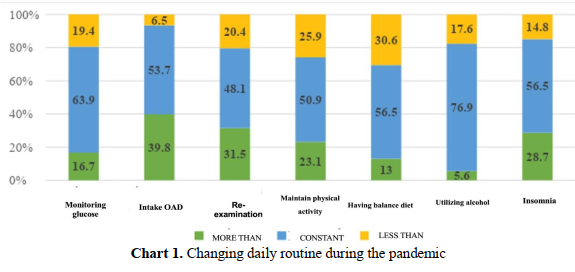
The bar chart 1 reveals the level of changing the daily routine of patients during the surveyed time. In general, during the pandemic, the patient daily routine changed in a positive direction. Most participants maintained and were more careful when taking the drug (93.5%). The figures for re- examination and self-monitoring of blood glucose also reached approximately 80%. About a quarter of patients decreased the time of doing exercise and 30.6% indicated less adherence to a balanced diet. Only 5.6% of patients consumed more alcohol but 28.7% of patients had insomnia.
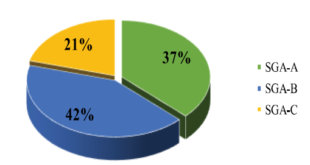
The tables 3 gives information on the prevalence of anxiety and stress as well as diabetes distress in participants in this study. The mean SAVE-6 score was 8.9 ± 6.3, with 25.9% of patients screened positive for anxiety and stress. Meanwhile, the prevalence of distress based on the DDS-2 scale (moderate and high distress) was significantly higher at 63% and the mean score was 2.25 ± 1.11. The mean score for changing daily routine was 5.8 ± 1.0.
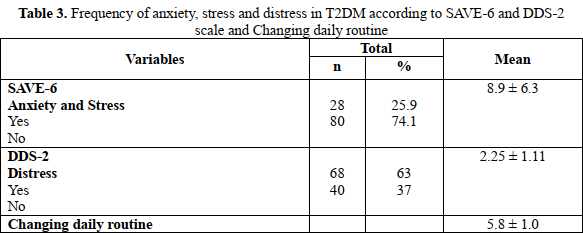
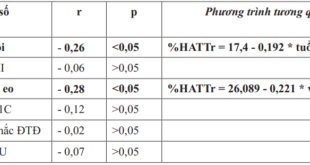
Table 4 presents the prevalence of anxiety, stress and distress in accordance with the distribution of some demographic and clinical characteristics. The prevalence of anxiety and stress was found higher in patients who had hypoglycemia (p= 0.034) but significantly decreased in patients who had higher education status (p= 0.021). Meanwhile, the proportion of distress diabetes was also higher in abdominal obesity patients (p= 0.01), those with anxiety regarding the virus (p< 0.001) and high of education status (p= 0.01).
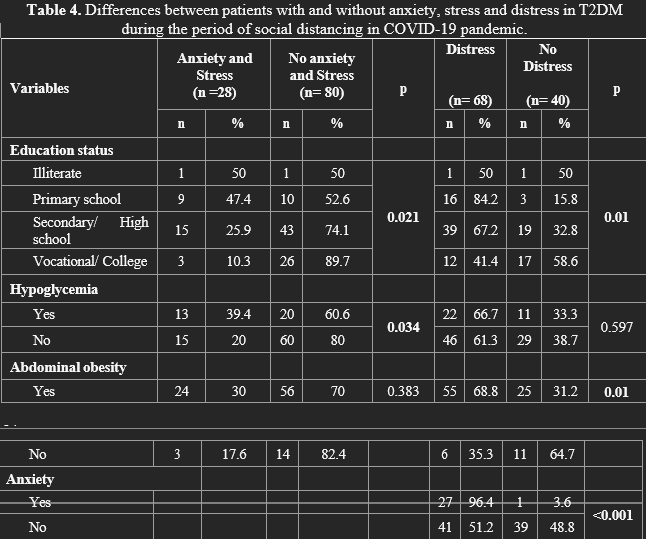
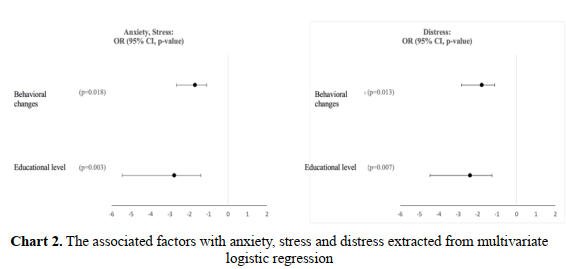
Chart 2 shows the associated factors with anxiety, stress and distress extracted from multivariate logistic regression. The model confirmed high education status was associated with decreasing anxiety and stress in an odds ratio (OR) of 95% CI 2.39 (1.26- 24.0) while changing daily routine in a positive direction also reduced by 1.79 the risk of psychological disorders with 95% CI (1.13- 2.85).
4. DISCUSSION
Our study maps overall mental health among T2DM in the period of social distancing during the COVID-19 pandemic in the central area of Vietnam. The prevalence of anxiety, stress and distress in participants in the surveyed time was high, marked at 25.9% and 76.2%, respectively, with several factors associated with those disorders. These results are equivalent to the proportion of a systematic review of thirty-seven articles collected from databases of six various libraries ( CINAHL, Cochrane, LILACS, Medline, SciELO, and Scopus) with a total 13,932 diabetes patients in several countries as well as scales which showed 23% T2DM patients had anxiety and 79% had distress in the period of the COVID- 19 pandemic [31].
Multiple studies performed prior to the COVID-19 pandemic showed that the prevalence of anxiety and distress in T2DM was 18% and 42.1%, respectively. This proportion proved a remarkable increase in psychological disorders during COVID time.
In comparison with other groups of diseases during the pandemic, the prevalence of anxiety and stress according to the SAVE-6 scale in cancer patients on Myung Hee Ahn’s study (49.8%) [28] [11], and in the general population in Seockhoon Chung’s study (49.7%) [29], there was a decrease of approximately a half in the figure of anxiety and stress in our study. The characteristics of diseases, sample size, healthcare system, and education status could explain these differences. In addition, we enrolled our sample in the time when Da Nang City had the fourth COVID-19 wave and the citizens, although complying with lockdown rules, were not on a stringent quarantine.
Our study revealed two independent factors for anxiety and stress: education status, with OR = 2.77 (CI 95%: 1.4 – 5.46), and level of changing daily routine with OR = 1.71 (95% CI: 1.1 – 2.66). Similarly, Kim Hae Ran’s study [32] showed that physical activity and getting sufficient sleep reduced stress with ORs of 1.35 and 2.21, respectively. Increased consumption of junk food, fast food, alcohol and smoking were also factors increasing stress in patients, with OR 1.8; 1.5; 2.22, and 2.17, respectively.
Regarding diabetes distress during the COVID-19 pandemic, according to the DDS-2 scale, the prevalence of distress in participants was 63%, lower than in Iran (76.2%) in a similar study by Maryam Peimani [33]. Although, our result was higher than several types of research in Vietnam as well as others countries in Southeast Asia. For example, 12.5% of VanBang Nguyen’s study in VietNam
[15] or 23.6% in another study was surveyed in the South of Vietnam [10], even though only 8.9% of participants had moderate to high levels of distress in Thailand [24].This information demonstrated the significance and negative effects of the virus on psychological disorders among the citizens. Our study highlights that high education level, abdominal obesity (p=0.01), and anxiety regarding the virus (p<0.001) increased the level of distress.
Multivariate analysis showed that education level and level of changing daily routine were also independent factors that impacted distress in diabetes patients, with OR 2.39 (CI95%: 1.27 – 4.46), and 1.79 (CI95%: 1.13 – 2.85). In
Egypt, a study by Sayed Ahmed using the PAID scale to assess distress among diabetes patients, indicated that the associated factors were marital status, illiteracy, unemployment, low income and comorbidities [27]. Although impacted factors for diabetes distress during the COVID-19 pandemic are not entirely similar across studies in different countries, overall, education status, anxiety regarding the virus, and unhealthy routine can increase the prevalence and level of distress diabetes.
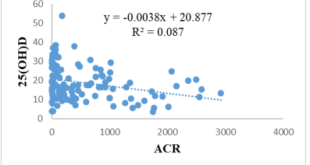
Our study also assessed the relationship between anxiety, stress and distress with duration diabetes and medicines treatment but there were not significantly associated with the level of psychological disorders. Poor control HbA1c, complications and comorbidities showed the resemble results. Although, previous studies reported that there was an influence of these factors on the level of psychological disorders. Since it is necessary to evaluate the bidirectional impact of metabolic control on mental health.
Our study also has several limitations. This study may not illustrate the whole picture of psychological disorders among Vietnamese diabetes patients throughout the nation. Our study was not conducted at the peak of the pandemic outbreaks also contributed to this limitation. Some essential variables were not identified in this study as a factor affecting of level anxiety, stress and distress among participants.
4. CONCLUSION
This study highlights a high prevalence of distress among people with diabetes during the COVID-19 pandemic, and associated anxiety of high-risk groups, and virus complications as well as education level and changing daily routine could help decrease the level of anxiety and stress of COVID-19.
Thus, our findings could be useful in emphasizing the importance of giving correct information and maintaining routine in a positive direction to support diabetes patients manage their anxiety and distress and reduce their psychological problems.
REFERENCES
1.(2019) “IDF Congress 2019: Shaping the future of diabetes”. Diabetes Res Clin Pract, 158, 107954.
2. Association American Diabetes (2022) “Standards of Medical Care in Diabetes- 2022 Abridged for Primary Care Providers”. Clin Diabetes, 40 (1), 10-38.
3. S. K. Brooks, R. K. Webster, L. E. Smith, L. Woodland, S. Wessely, N. Greenberg,G. J. Rubin (2020) “The psychological impact of quarantine and how to reduce it: rapid review of the evidence”. Lancet, 395 (10227), 912-920.
4. I. Cancarevic, M. Nassar, A. Daoud, H. Ali, N. Nso, A. Sanchez, A. Parikh, A. Ul Hosna, B. Devanabanda, N. Ahmed, K. M. Soliman (2022) “Mortality rate of COVID- 19 infection in end stage kidney disease patients on maintenance hemodialysis: A systematic review and meta-analysis”. World J Virol, 11 (5), 352-361.
5. D. Cucinotta, M. Vanelli (2020) “WHO Declares COVID-19 a Pandemic”. Acta Biomed, 91 (1), 157-160.
6. O. Dyer (2020) “Covid-19: Pandemic is
having “severe” impact on noncommunicable disease care, WHO survey
finds”. BMJ, 369, m2210.
7. A. S. Fauci, H. C. Lane, R. R. Redfield (2020) “Covid-19 – Navigating the Uncharted”. N Engl J Med, 382 (13), 1268-1269.
8. L. W. Holaday, C. R. Oladele, S. M.Miller, M. I. Duenas, B. Roy, J. S. Ross (2022) “Loneliness, sadness, and feelings of social disconnection in older adults during the COVID-19 pandemic”. J Am Geriatr Soc, 70 (2), 329-340.
9. L. Hou, F. Long, Y. Meng, X. Cheng, W. Zhang, R. Zhou (2021) “The Relationship Between Quarantine Length and Negative Affect During the COVID-19 Epidemic Among the General Population in China: The Roles of Negative Cognition and Protective Factors”. Front Psychol, 12, 575684.
10. G. Huynh, T. T. Tran, T. H. T. Do, T. T. D. Truong, P. T. Ong, T. N. H. Nguyen, L. A. Pham (2021) “Diabetes-Related Distress Among People with Type 2 Diabetes in Ho Chi Minh City, Vietnam: Prevalence and Associated Factors”. Diabetes Metab Syndr Obes, 14, 683-690.
11. H. Kim, H. Kim, H. J. Lee, E. Cho, S. J. Koh, O. Ahmed, S. Chung (2022) “The Validation Study of the Stress and Anxiety to Viral Epidemics-6 Scale Among
 Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam
Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam