COMPLICATIONS AND ITS ASSOCIATION WITH SLEEP QUALITY IN THE ELDERLY DIABETIC PATIENTS
Nguyen Thi Thu Huong1,2, Nguyen Trung Anh1,2
1 National Geriatric Hospital, 2 Hanoi Medical University
DOI: 10.47122/vjde.2021.48.4
ABSTRACT
Background: Sleep disorders are commonly seen in type 2 diabetic patients. However, there is not much research about the association of diabetic complications and poor sleep quality. Objectives: To evaluate diabetic complications and to find out which diabetic complications are associated with poor sleep quality in older diabetic patients treated at National Geriatric Hospital. Methods: A cross-sectional study on 178 older diabetic patients treated at National Geriatric Hospital from March to October, 2020. Quality of sleep was assessed using the Pittsburgh Sleep Quality Index. Results: 93 patients (52.2%) had peripheral nerve complications. 50% patients had diabetic retinopathy. There were 86 patients (48.3%) had experienced hypoglycemia in the last 3 months. The prevalence of diabetic neuropathy, cerebral vascular disease, cardiovascular disease, peripheral artery disease and foot complication were 12.9%; 12.9%; 9%; 8.4% and 7.3%, respectively. 19.1% patients didn’t have any complications of diabetes. Patients with diabetic retinopathy and cerebral vascular disease had a significantly higher rate of poor sleep quality compared with the group without these complications. There were no significant association between diabetic nephropathy, cardiovascular disease, peripheral nerve complication, foot complication, hypoglycemia and sleep quality. Conclusion: This study showed that older diabetic patients had many complications. Diabetic retinopathy and cerebral vascular disease were higher in the poor sleep quality group.
Keywords: sleep quality, diabetic complication, older patients.
Main correspondence: Nguyen Trung Anh Submission date: 20th April 2021
Revised date: 26th April 2021 Acceptance date: 26th May 2021
Email: [email protected] Tel: 0903480774
1. INTRODUCTION
Type 2 diabetes (T2D) is a chronic condition of public health concern due to its high morbidity and mortality and significant loss of quality of life. Diabetes prevalence increases with age. According to the International Diabetes Federation Atlas 9th edition 2019, among 704.4 million adult population (65-99 years), the estimated number of people with diabetes is 135.6 million (19.3%); and if this trend countries, the number of people above 65 years with diabetes will be 195.2 million in 2030 and 276.2 million in 2045 [1]. Good blood glucose control in diabetics promotes the effectiveness of the treatment process as well as prevents severe complications.
Sleep disorders are commonly seen in T2D patients because of the disease itself, its complications and other comorbidities. The prevalence of poor sleep quality among T2D patients’ ranges from 45% to 70% [2]. T2D, in addition to causing direct sleep disturbances as a result of nocturia, polyuria, has also been associated with diabetic complications and several chronic illness as obstructive sleep apnea, hypertension and depression which can impair sleep and quality of life. The patient may not bring the sleep issues during their visit to healthcare providers, with acute issues taking precedence during their visit. It is important for the health care providers treating the patient with DM to address their sleep issues and the impaired quality of life due to inadequate and fragmented sleep, as it may severely affects their recovery, control of diabetes as well as quality of life [3].
Specifically, there are currently studies on sleep disorders in some populations, but in Vietnam there are very few studies on the association between sleep quality and diabetic complication in older patients with T2D. Thus, the aims of the present study were to evaluate diabetic complications and to find out which diabetic complications are associated with poor sleep quality in older diabetic patients in National Geriatric Hospital.
2. SUBJECTS AND METHODS
2.1. Subjects
Older diabetic patients aged 60 years old and over, being treated at National Geriatric Hospital from March to October, 2020. Patients were excluded from this study if they had some conditions such as mental disorder; severe cognitive impairment or patients were inability to communicate.
2.2. Study design: the study was a cross- sectional study with convenience sampling. The sample size was calculated using the formula.
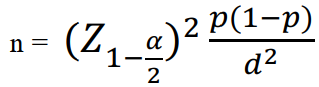
n: study sample size;
α: statistical significance level, with α = 0,05; (Z1- α/2) = 1,96
p = 0.473 (Prevalence of sleep disturbance among type 2 diabetes patients in Zhu’s study in 2014) [4].
d = expected error (d = 0.075).
From the formula, the estimated sample size was 170 diabetic patients. Finally, the number of patients in our study was 178.
2.3. Variables
- General information: age,
- Quality of sleep was assessed using the Pittsburgh Sleep Quality Index (PSQI) [5]:
The PSQI score is calculated by total points of seven components:
- Subjective sleep quality
- Sleep latency
- Sleep duration
- Habitual sleep efficiency
- Sleep disturbances
- Use of sleep medication
- Daytime dysfunction over the last month Maximum of a normal sleep is less than 9. If result is more than or equal 9, the participant will get poor sleep.
- Diabetic complications were collected using medical records at the hospital (based on clinical and subclinical symptoms and diagnosed of medical doctors):
+ Diabetic retinopathy
+ Diabetic nephropathy
+ Cerebral vascular disease
+ Cardiovascular disease
+ Peripheral artery disease
+ Peripheral nerve complications
+ Foot complication
+ Hypoglycemia in the last 3 months
2.4. Tools and data collection method
Data were collected by using designed questionnaire and medical record at National Geriatric Hospital.
2.5. Data processing and data analysis
The process of data coding, entry into Redcap and analysis was done by using Statistical Package for Social Science (SPSS) software (version 20). Descriptive statistics were adopted to examine characteristic data: frequency, percentage, mean. Inferential statistics was done to perform comparisons between groups: t-Test, Chi-square. Statistical significance was accepted at the 95% confidence level (p<0.05).
3. RESULTS
After evaluating diabetic complications and its association with sleep quality among 178 type 2 diabetic older patients at National Geriatric Hospital, we found the results of statistic analyzing as follows:
3.1. Subjects’ characteristics
The mean aged of participants was 73.5 years old (SD=8.0) and the group of above or equal 70 years old was majority (66.3%). Almost participants was female (57.3%). Participants in this study had average duration of diabetes was 9.09±7.84 (year).
According to the PSQI scale, there were 120 participants (67.4%) had poor sleep, while only 58 participants (32.6%) had normal sleep.
3.2. The percentage of diabetic complications in older patients
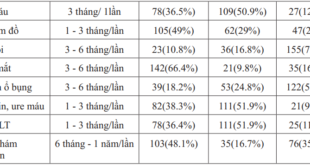
Table 1. Diabetic complications in older patients
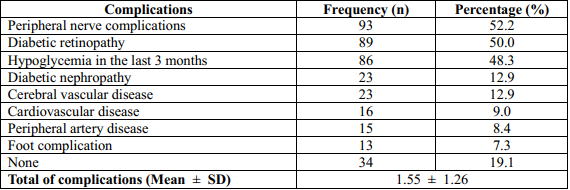
93 patients (52.2%) had peripheral nerve complications. A half of participants had diabetic retinopathy. There were 86 patients (48.3%) had experienced hypoglycemia in the last 3 months. The prevalence of diabetic neuropathy and cerebral vascular disease that patients have was the same, 12.9% (23 patients). The number of patients had cardiovascular disease, peripheral artery disease and foot complication were 16, 15 and 13 patients, respectively (9%, 8.4% and 7.3%, respectively). Thirty-four patients (19.1%) didn’t have any complications of diabetes. The mean of complications that they have was 1.55 complications (SD=1.26).
3.3. Association between diabetic complications and sleep quality
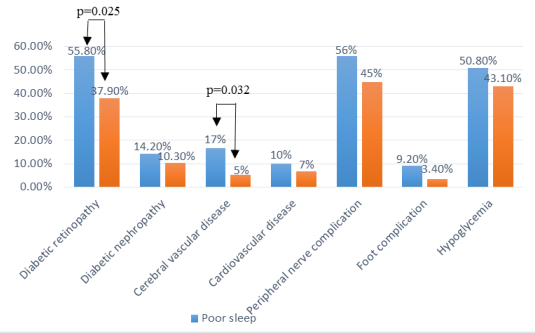
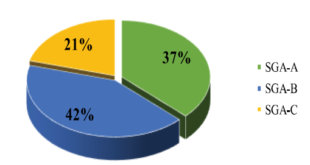
Figure 1. Association between quality of sleep and diabetic complications
There was significant association between quality of sleep and diabetic retinopathy and cerebrovascular disease with p = 0.025 and p = 0.032, respectively. Among patients with diabetic retinopathy, the percentage of patients had poor sleep quality was higher than the ones had normal sleep quality (55.8%>37.9%). And, among patients had cerebral vascular disease, the percentage of patients had poor sleep quality was higher than the ones had normal sleep quality (17%>5%). There were no significant association between diabetic nephropathy, cardiovascular disease, peripheral nerve complication, foot complication, hypoglycemia and sleep quality, p>0.05.
Table 2. Association between the number of diabetic complications and quality of sleep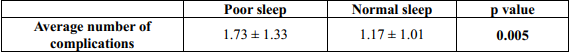
In addition, there was significant difference of the mean of total complications between 2 groups of diabetes, the patients with poor sleep quality had higher the average of total complications than the ones with normal sleep quality (1.73±1.33 and 1.17±1.01 respectively, p=0.005).
4. DISCUSSION
This study was conducted to evaluate diabetic complications and its association with sleep quality in older patients. Our results showed that diabetic retinopathy and peripheral nerve complications had highest percentage, 50% and 52.2% respectively. The percentage of diabetic retinopathy in this study was higher than percentage of Japanese research (50% > 23.6%) [6]. The percentage that patients had diabetic nephropathy and cerebral vascular diseases in this study was equal, 12.9%. It was similar with nephropathy percentage (12.4%) but lower than neuropathy percentage (43.3%) in Japanese research above [6]. The percentage of neuropathy in this study was lower than percentage in Chinese research also (12.9% < 43%) [7]. The percentage of hypoglycemia in this study was higher than percentage in Ha Dong traditional hospital research, 48.3% and 20.6% [8] respectively. The difference in result can be from difference of sample size between studies. Besides, this study observed that the mean of total complications was 1.55 ± 1.26, it was higher than Luyster’s research in 345 type 2 diabetic patients (0.72±0.97) [9]. This reason may be explained by different research subject and sample size.
These results showed that there were statistical significances different between two groups of sleep quality and the mean of total complications, p=0.005. Previous research among three hundred patients with type 2 diabetes (mean age 63.9 years) in the University of Pittsburgh, school of nursing in 2011 shown that there was no significant difference between two groups of sleep quality and the mean of total complications, p=0.13>0.05 [9]. It was opposite with this study. The difference in result between this study and those studies can be explained by the difference of populations and sample sizes.
Among diabetic complications, diabetic retinopathy and cerebral vascular disease were statistical significant association with quality of sleep, p=0.025 and p=0.032 respectively. To date, there were some studies have reported on the association between sleep duration and diabetic retinopathy [10–12]. The first of these cross-sectional studies found no associations between short or long sleep duration with diabetic retinopathy on multivariate logistic regressions in Indian persons with diabetes [12]. In other studies of 1,670 Korean and 1,220 Chinese adults with diabetes, long, but not short, duration of sleep was associated with higher odds of diabetic retinopathy on multivariable analysis [10,11]. Our results showed that there were no statistical significance association between sleep quality and diabetic nephropathy, cardiovascular disease, peripheral nerve complication, diabetic foot and hypoglycemia, p>0.05. This result was similar with research in 220 patients with type 2 diabetes in China in 2014, it shown that there was no statistical significance association between quality of sleep and diabetic foot, p=0.161 [7]. The difference in result between this study and those studies can be explained by the difference of sample size, range of age and cross-sectional study.
5. CONCLUSIONS
This study showed that older diabetic patients had many complications. Diabetic retinopathy and cerebral vascular disease were higher in the poor sleep quality group. Other diabetic complications showed no significant difference in both groups.
REFERENCES
- International Diabetes Federation, (2019). “IDF Diabetes Atlas – ninth edition”.
- Yücel Ş., Kocaçal E., and Ak İ. (2014). “Investigation of sleep quality, quality of life, anxiety and depression in patients with diabetes mellitus”, Int J Diabetes Dev Ctries, 35, 39–46.
- Surani S, Brito V, Surani A, Ghamande S., (2015). “Effect of diabetes mellitus on sleep quality”, World J Diabetes. 2015;6(6):868- 873. doi:10.4239/wjd.v6.i6.868
- Zhu B.-Q., Li X.-M., Wang D., et al. (2014).” Sleep quality and its impact on glycaemic control in patients with type 2 diabetes mellitus”, Int J Nurs Sci, 1(3), 260– 265.
- Smyth C. (2003). “The Pittsburgh Sleep Quality Index. (Try This: Best Practices in Nursing Care to Older Adults from The Hartford Institute for Geriatric Nursing)”, MedSurg Nurs, 12(4), 261–263.
- Sakamoto R., Yamakawa T., Takahashi K., et al. (2018). “Association of usual sleep quality and glycemic control in type 2 diabetes in Japanese: A cross sectional study”, Sleep and Food Registry in Kanagawa (SOREKA). PLOS ONE, 13(1), e0191771.
- Qiu L, Sautter J, Liu Y, Gu , (2011). “Age and gender differences in linkages of sleep with subsequent mortality and health among very old Chinese”, Sleep Med. 2011;12:1008–17.
- Nguyễn Thị Thùy Dương (2019), “Đánh giá rối loạn giấc ngủ trên bệnh nhân đái tháo đường cao tuổi tại bệnh viện Y học cổ truyền Hà Đông”, Đại học Y Hà Nội.
- Luyster F.S. and Dunbar-Jacob J. (2011). “Sleep Quality and Quality of Life in Adults With Type 2 Diabetes”, Diabetes Educ, 37(3), 347–355.
- Jee D, Keum N, Kang S, Arroyo JG., (2017). “Sleep and diabetic retinopathy”, Acta Ophthalmol. 2017;95(1):41–7. pmid:27473575.
- Meng LL, Liu Y, Geng RN, Tang YZ, Li DQ., (2016). “Association of diabetic vascular complications with poor sleep complaints”, Diabetol Metab Syndr. 2016;8:80. pmid:27980688.
- Raman R, Gupta A, Venkatesh K, Kulothungan V, Sharma , (2012). “Abnormal sleep patterns in subjects with type II diabetes mellitus and its effect on diabetic microangiopathies: Sankara Nethralaya Diabetic Retinopathy Epidemiology and Molecular Genetic Study (SN-DREAMS, report 20)”, Acta Diabetol. 2012;49(4):255–61. pmid:21113729.
 Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam
Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam