STUDY OF SERUM HIGH SENSITIVITY C –REACTIVE PROTEIN
(hs-CRP) AND RISK FACTORS IN TYPE-2 DIABETIC PATIENTS
Nguyễn Văn Mùi*, Vũ Bích Nga**
ABSTRACTS
Background: Serum levels of high-sensitivity C-reactive protein (hs-CRP) have been found to be a strong predictor for increased cardiovascular disease risk associated with type 2 diabetes. Objective: The aim of this study was to assess the association of hs-CRP with other risk factors in type 2 diabetic patients such as diabetes duration, BMI, hypertension, glycemic control, dyslipidemia, and microalbuminuria.Patients and Methods: A cross-sectional population-based study of 79 type 2 diabetic patients admitted to the Endocrinology department of Bachmai hospital and Hanoi Medical University Hospital. Medical history, physical examination, and laboratory findings of these subjects were evaluated in terms of the factors influencing hs-CRP level.: Serum hs-CRP level was significantly higher in type 2 diabetic patients with long duration time with diabetes, BMI (body mass index) > 23, high WHR (waist-to-hip ratio),high blood pressure; high HbA1c levels and with microalbuminuria. There was a strong positive correlation between serum hs- CRP with HbA1c and microalbuminuria. Conclusions:In type 2 diabetic patients,theincreaseofserumhs-CRP concentration was correlated with long duration of diabetes; with high BMI, WHR, blood pressure, HbA1c, LDL-C, and with the presence of microalbuminuria. The current study demonstrates a strongest positive correlation of serum hs- CRP with HbA1c and microalbuminuria.
Key word: hs-CRP, risk factors, type 2 diabetic patients.
Main correspondence:Nguyen Van Mui
Submission date: 9 Feb 2017
Revised date: 21 Feb 2017
Acceptance date: 15Mar 2017
I. Introduction
Diabetes is an important chronic disease which incidence is globally increasing and now considered as an epidemic [1].
Individuals with diabetes and with chronically poor metabolic control can experience microvascular and macrovascular complications leading to a significant burden for them and for society. Cardiovascular diseases (CVD) are the most prevalent cause of mortality and morbidity among people with type 2 diabetic patients. The rate of mortality due to heart disease and stroke in adult people with diabetes was two to four times higher than those without diabetes.
The underlying mechanisms that cause accelerated atherosclerosis in patients with diabetes and consequently an increased prevalence of CVD are poorly understood.
The purpose of this paper is to describe the association between poor glycemic control, oxidative stress, markers of insulin resistance, and of low-grade inlammation that have been suggested as putative factors linking these two conditions [3], [4], [5].
Several studies have linked high level of serum hs-CRP to an increased risk of cardiovascular events, including myocardial infarction, and have identified serum hs-CRP as a predictive biomarker of cardiovascular risk and cardiovascular mortality in various patient populations, including diabetic patients [6], [7]. In diabetic patients with an acute myocardial infarction and elevated hs-CRP level, hospital outcome is poorer than in nondiabetic patients with an acute myocardial infarction [8] without elevated hs-CRP .
The link between serum hs-CRP and the other risk factors in diabetic patients such as poor glycemic control, obesity, hypertension, and dyslipidemia still remain to be fully elucidated.
2. Patients and Methods
2.1 Study Design
The study design was cross-sectional. A total of 79 type 2 diabetic patients admitted to the Endocrinology Department of Bachmai Hospital and Hanoi Medical University Hospital from Feb to Oct 2014. The subjects were of both sexes, in the age group of 40-78 years old. Detailed interview using a structured questionnaire were performed with physical examinations, and laboratory findings of these subjects were done comprising serum hs-CRP; HbA1c, microalbuminuria, lipid profile. T2D was diagnosed in accordance with ADA 2012 criteria [9]. Patients with concurrent acute illnesses including infectious diseases within the past 1 week, malignancy, and active immunological diseases; medical history of clinical cardiovascular disease; tuberculosis, pregnancy, lactation, using corticosteroids or confounding factors for proteinuria, renal insufficiency; type 1 diabetes patient, pregnant women, children; adolescents were excluded. All subjects with serum hs-CRP value greater than 10 mg/liter have also been excluded from analysis.
BMI was calculated and classified by WHO criteria
High BP was diagnosed in accordance with JNC VII
2.2 Blood Collection & Biochemical Assay
Blood samples were taken in the morning after 8 to 12 hours overnight fast. Samples were collected in sterile tubes, and sent to the hospital laboratory departments within under 1 hour.
The glycosylated hemoglobin (HbA1C) concentration was measured by ion exchange chromatography. Serum total cholesterol, HDL-cholesterol (HDL-C), serum triglyceride and LDL-cholesterol (LDL-C) were estimatedby standard methods. Plasma levels of hs-CRP were measured using Randox kit, United Kingdom (HITACHI 717 machine). Urinary albumin excretion assay: A morning sample quantitative determination of microalbumin in urine. Data for continuous variables are expressed as median and comparison with student T-test.Differences in distribution among the three categories were assessed using test.
2.3Results
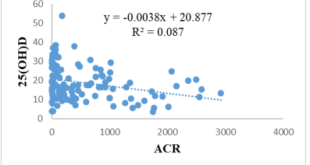
Table 1 . The clinical and biochemical characteristics in relation to serum hs-CRP
Figure 1. Correlation between hs-CRP and HbA1c in patients with diabetes mellitus.
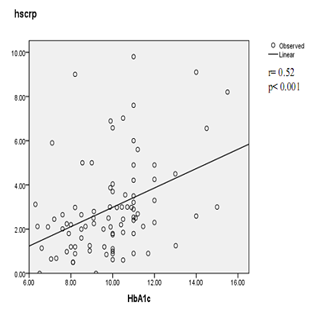
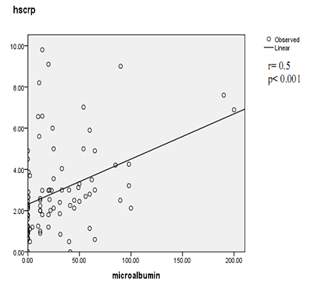
Figure 2. Correlation betweenhs-CRP and urinary albumin excretion in patients with diabetes mellitus
2.4 Discussion
The clinical and biochemical characteristics in relation to hs-CRP of the study group were shown on the table 1. We observed that the hs-CRP level was significantly higher in subjects with obesity or overweight, high WHR, or patient with high blood pressure. hs-CRP level was also significantly higher in diabetic patients with high LDL-C as compared to diabetic patient with normal LDL-C (p<0.05). Several earlier studies have shown the similar results. In a study by Safiullah Amanullah, Abdulla Jarari et al. in 2010, subjects with abnormal hs-CRP had higher proportion of hypertension, obesity, hypercholesterolemia [10]. A study reported by Paul M Ridker, Julie E. Buring et al in 2003 showed that serum CRP level was significantly higher among type 2 diabetic patients who had any component of the metabolic syndrome: obesity, dyslipidemia, high blood pressure [11]. Several explanations are possible for the apparent association between CRP and BMI, dyslipidemia. First, individuals with obesity are at increased risk for various chronic diseases, such as cardiovascular diseases, insulin resistance condition which are also characterized by elevated CRP concentration [6], [12]. Interestingly, hs-CRP level in type 2 diabetic patients who had microalbuminuria was increased many times than patients without microalbuminuria. Study of Mohd. Idrees Khan el al in 2012 [13], and Marije van der Velde et al in 2012 [14], have showed the similar results: hs-CRP level was higher among subjects with elevated albuminuria versus subjects with normoalbuminuria.
This study also showed a weak correlation between UAE and inflammatory parameter in type 2 diabetic patients at an early stage of diabetic nephropathy. Inflammatory markers in early diabetic nephropathy in patients with type 2 diabetes were elevated. In this study, we compared the serum hs-CRP level with different levels of HbA1c. For each level of HbA1c, and the elevation of hs-CRP level was as follows: <7%, 1.6 ± 1.17mg/l ; 7– 8.9%, 2.3± 1.96mg/l; 9 –10.9%, 2.7 ± 1.73mg/l; and ≥ 11%, 4.0 ± 2.37mg/l. The current study demonstrates that higher HbA1c is significantly associated with elevation of CRP. These results imply a significant relation between inflammation and glycemic control in people with type 2 diabetes. The similar results were observed in the study of M. S. Roopakala et al in 2012 [15]; and of Dana King et al in 2003 [16]. On analysis of the correlation between hsCRP level and HbA1c, and microalbuminuria as showed in figure 1 and figure 2, we found a positive correlation between hs-CRP level and HbA1c (r= 0.52; p< 0.001) and a positive correlation between hs-CRP level and microalbuminuria (r= 0.5; p< 0.001). The positive correlation of hs-CRP with HbA1c was also observed in the previous study. Mohd. Idrees Khan, Kauser Usman et al reported in 2012 that glycemic control (HbA1c) and microalbuminuria were the major correlates of hs- CRP level in type 2 diabetic patients [13]. These results suggest that the determination of serum hs-CRP levels may help in early intervention and prevention of further complications in diabetic patients.
2.5. Conclusion
In type 2 diabetic patients, an elevated serum hs-CRP level was positively associated with the length of time with diabetes, overweight/obesity, high blood pressure, poor glycemia control, microalbuminuria and dyslipidemia. The strongest positive correlation of serum hs- CRP level was observed with HbA1c (r= 0.52; p< 0.001) and with microalbuminuria (r= 0.5; p< 0.001).
REFERENCES
- IDF DIABETES ATLAS, 5th edition, 2012 update.
- WHO (2011), “Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia”, report of a WHO/IDF consultation, 2006.
- Coson (2006), “Physiopathologie des complications du diabète”, Réalités Cardiologiques, N° 213 – Cahier 1, Janvier 2006
- Jenny E. Kanter, Michelle M. Averill, Renee C. LeBoeuf et al (2008), “Diabetes-Accelerated Atherosclerosis and Inflammation”, 2008; 103: e116-e117 Circ Res.http://circres.ahajournals.org/content/103/8/e116
- S Chaikate1, T Harnroongroj, Y Chantaranipapong (2006). “C-reactive protein, Interlekin-6, and tumor necrosis factor- α level in overweight and healthy adults”, Southeast Asia J Trop Med public health, Vol 37 No. 2 March 2006.
- Paul M Ridker PM, Buring JE, Cook NR, et al,“C-reactive protein, the metabolic syndrome, and risk of incident cardiovascular events: an 8-year follow-up of 14 719 initially healthy American women. Circulation. 2003; 107: 391–397. Abstract/FREE Full Text
- David M. Capuzzi et al (2007), “C – reactive protein and Cardiovascular Risk in the Metabolic Syndrome and Typ 2 Diabetes: Controversy and Challenge”, Volume 25, Number 1, 2007 16, CLINICAL DIABETES.
- Renu Virmani et al (2002), “Elevated CRP values and atherosclerosis in sudden coronary death”, Circulation, 105, pp. 2019-29.
- International Diabetes Federation (2012), “Global Guideline for Typ 2 Diabetes”
- Safiullah Amanullah et al (2010), “Association of hs-CRP with Diabetic and Non-diabetic individuals”, Jordan Journal of Biological Sciences, Volume 3, Number 1, January 2010 ISSN: 1995-6673, Pages 7–12
- Ridker PM, Rifai N, Rose L, et al. “Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events”. N Engl J Med. 2002; 347: 1557–1565. CrossRefMedline
- Earl S. Ford (1999), “Body Mass Index, Diabetes, and C-Reactive Protein among U.S. Adults”, Diabetes Care 2 2:1 9 7 1–1977, 1999.
- Idrees Khan, Kauser Usman et al (2012), “Association of Hs-CRP and HbA1C with Microalbuminuria in Type-2 Diabetic patients in North India”. Biomedical Research 2012; 23 (3): 380-384
- Marije van der Velde, Aminu K. Bello, Auke H. Brantsma et al (2012) “Do albuminuria and hs-CRP add to the International Diabetes Federation definition of the metabolic syndrome in predicting outcome?” Nephrol Dial Transplant: 1–9 doi: 10.1093/ndt/gfr634
- S. Roopakala et al (2012), “Evaluation of High Sensitivity C-reactive Protein and Glycated Hemoglobin Levels in Diabetic Nephropathy”, Saudi J Kidney Dis Transpl 2012;23(2):286-289
- Dana E. King, Thomas A. Buchanan, et al, (2003), “C-Reactive Protein and Glycemic Control in Adults with Diabetes”, Diabetes care, 26 (5).
 Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam
Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam