CARDIOVASCULAR RISK FACTORS IN TYPE 2 DIABETIC OUTPATIENT ACCORDING TO THE RECOMMENDATIONS OF ESC-EASD 2019
Huynh Le Thai Bao1,*
1. Faculty of Medicine, Duy Tan University, Da Nang, Vietnam
DOI: 10.47122/vjde.2021.48.3
ABSTRACT
Cardiovascular risk factors in type 2 diabetic outpatient according to the recommendations of ESC-EASD 2019
Objectives: To evaluate some cardiovascular risk factors in type 2 diabetes outpatient receiving treatment at Cu Jut district general hospital, Dak Nong province in 2020 according to the recommendations of ESC-EASD 2019. Methodology: The study used a descriptive cross-sectional design with a continuous sampling method during the study to evaluate some cardiovascular risk factors in patients with type 2 diabetes mellitus treatment. reside at the medical center of Cu Jut district, Dak Nong in 2020 according to the recommended treatment recommendations of ESC-EASD 2019. Each patient in the study sample was examined and given the contents of the prepared questionnaire. Each was designated any required subclinical processes as necessary. Results obtained: Target characteristics of controlling some cardiovascular risk factors in diabetic patients according to ESC – EASD 2019 guidelines: BMI ratio over 23 kg / m2 is 35.3%, round rate increase abdomen was 76.05%, incidence of uncontrolled blood pressure was 47.3%, total cholesterol was 49.3%, tryglicerid was 50.7%, HDL-C was 34.7% and non-HDL-C was 54.6% and LDL-C was 82.8%.
Keywords: Type 2 diabetes, ESC – EASD 2019, cardiovascular risk stratification, cardiovascular disease, target organ damage.
Main correspondence: Huynh Le Thai Bao Submission date: 20th April 2021
Revised day: 26th April 2021 Acceptance date: 26th May 2021 Email: hlthaibao@gmail.com Tel: 0888838539
1. STATEMENT OF THE PROBLEM
In recent years, cardiovascular disease has always been the leading cause of death in the world. According to the World Health Organization (WHO) in 2016, every year about 17.9 million people die from cardiovascular disease, accounting for 31% of all deaths worldwide [6]. In Vietnam, according to WHO, the death rate from cardiovascular disease is also 31% [7] -. Therefore, the prevention of cardiovascular diseases helps to reduce the burden of disease on society. For effective prevention, it is essential to control the risk factors.
Of the above cardiovascular risk factors, diabetes is an important and independent risk factor. The prevalence of diabetes in the world is on the rise, with an estimated 60 million Europeans infected [9]. In East Asian countries, with lifestyles gradually becoming more similar to the West, the prevalence of diabetes continues to increase, up to 10% of the population as in China, India [9]. In Vietnam, up to 5.42% of people aged 30-69 years have diabetes. These figures pose a serious challenge for developing economies, as the cardiovascular complications of diabetes can cause premature death, disability, loss of work capacity, and socio-economic consequences. [1].
In 2019, ESC and EASD jointly launched the ” Guidelines on Diabetes, Pre-Diabetes and Cardiovascular Diseases” to provide guidance on the management and prevention of cardiovascular disease in those already suffering from disease or at risk of diabetes. These guidelines emphasize the development of ways to prevent and manage the impact of diabetes on cardiovascular disease. The guide also uses ESC 2016 cardiovascular risk stratification and includes new updates on individualization of cardiovascular risk factors treatment.
From the above reasons, we conducted this study to evaluate some cardiovascular risk factors in patients with type 2 diabetes in outpatient treatment at Cu Jut district health center, Dak Nong by 2020 according to Treatment recommendation goals of the ESC- EASD 2019.
2. SUBJECT AND METHODOLOGY Research location and time: Department of
Examination and Emergency, Medical Center of Cu Jut district, Dak Nong province from January 2020 to June 2020.
Subjects: All patients with confirmed diagnosis of type 2 diabetes who came for examination and follow-up examinations. Meet the following criteria:
• Sampling criteria
Patients diagnosed with diabetes by fasting glucose according to the standards of the American Diabetes Association in 2017 [10]:
-When there are clinical symptoms of diabetes (heavy drinking, excessive urination, weight loss) or acute decompensation with ≥ 1 test:
+ Fasting glucose: ≥ 7.0 mmol / l.
+ HbA1 C ≥ 6.5%.
Any blood sugar ≥ 11.1mmol / l.
-When there are no clinical symptoms of diabetes and acute decompensation, based on tests:
+ Fasting glucose: ≥ 7.0 mmol / l, ≥ 2 times at least 1 day apart.
+ HbA1 C ≥ 6.5%, ≥ 2 times at least 3 months apart.
+ Fasting glucose ≥ 7.0 mmol / l and HbA1 C ≥ 6.5%.
Previous diagnosis of diabetes
- Previously diagnosed with diabetes, currently taking diabetes medicine with any amount of blood
- Previously diagnosed with diabetes, dropped out of treatment and only meet requirements of fasting glucose or high
Diagnosis of type 2 diabetes
Onset is usually discreet;
- Blood sugar is usually stable even with lifestyle changes or non-insulin medications;
- Excluding type 1 diabetes and other special type
• Exclusion criteria:
- The patient does not agree to participate in the
- Patients with acute complications of diabetes.
Research Methods
Study design: Descriptive cross-sectional study.
Sampling: Survey the entire target population through consecutive sampling during the study period.
Standards used in research
- Identified cardiovascular disease: A cardiovascular disease that has been clinically or clearly identified, including: history of myocardial infarction, acute coronary syndrome, coronary revascularization, cerebral stroke and peripheral artery
- ESC 2016 stratification of cardiovascular risk factors for diabetic patients [12]:
Very high risk: Diabetic patients already suffering cardiovascular disease
+ Or other target organ damage (Proteinuria, renal failure when eGFR <30mL /min, left ventricular hypertrophy, retinopathy)
+ Or ≥ 3 main risk factors (age greater than 65, hypertension, dyslipidemia, smoking, obesity)
+ Or early onset diabetes with long duration (> 20 years)
High risk: Diabetes duration ≥ 10 years, no target organ damage + no other additional risk factors.
Average risk: Young (<50 years) patient with diabetes duration <10 years, with no other risk factors.
- The recommended treatment goals according to ESC Guidelines – EASD 2019 for diabetic patients [9]:
The ESC – EASD 2019 guidelines have many updates compared to the ESC – EASD 2016, in which the treatment recommendation goals are individualized:
– Target blood pressure: For patients ≤ 65 years old: The target systolic blood pressure is 130 mmHg, if tolerated it can be reduced to <130 mmHg but not <120 mmHg. For patients> 65 years of age, the target systolic blood pressure is between 130 mmHg and 139 mmHg. The target for diastolic blood pressure is <80 mmHg but not <70 mmHg.
Target blood fat: For average cardiovascular risk, target LDL-C <2.5mmol / L, for high cardiovascular risk, LDL-C <1.8 mmol / L, for heart risk very high circuit, LDL-C <1.4 mmol/ L. Other lipid indexes: Total cholesterol (TC) <4.5 mmol / L, Triglycerid <2.3 mmol / L, HDL-C> 1.0 mmol / L, non HDL – C <3.3 mmol/ L.
- Target blood sugar: fasting glucose <7.2 mmol / L, postprandial glucose <10 mmol / L, HbA1C <7%.
- Smoking: Stop required.
- Exercise strength: 30 – 45 minutes / day
- BMI: less than 23 kg / m2
- Waist circumference: <90 cm for men and <80 cm for women.
Data processing and analysis: Data entry using EpiData 3.1 software, data processing using R Studio 4.0 software. Values of quantitative variables are presented as mean ± standard deviation (Mean ± SD) or median and the minimum and maximum value when distributing the deviation. Qualitative data are presented as a percentage.
3. FINDINGS AND DISCUSSION
General characteristics of the research sample
During the implementation period, there were 150 subjects participating in our study.
The average age of the study sample is 60.06 ± 10.88. The age group with the highest proportion is the age group 50-59 with 31.3% and the age group 60-69 with 30.0%.
This result is similar to many studies. In the study of Nguyen Le Phuong Anh (2019) at the District 3 Hospital – Ho Chi Minh City, the two age groups accounting for the highest proportion are 60-69 years old with 34.9% and 50-59 years old with 27% [2].
In the study of Vien Van Doan (2012) at Bach Mai hospital, the age group accounting for the highest percentage is 50-60 years old with 41.2%, followed by the 60-70 years old group with 33.8%. It can be seen that the age group 50 – 70 years old always accounts for the highest proportion in the studies [5].
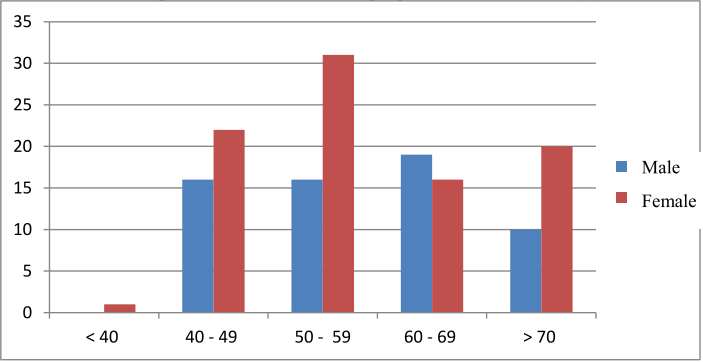
Chart 1. General characteristics of research sample
In our study, women account for 59.3% higher than men with 40.7%. This rate is similar to the study of Vien Van Doan (2012) with 59.8% female, 40.2% male and Nguyen Le Phuong Anh (2019) with 53% of females and 53% of men. accounting for 47% [2], [5]. Among the studies, the percentage of women is always higher than that of men.
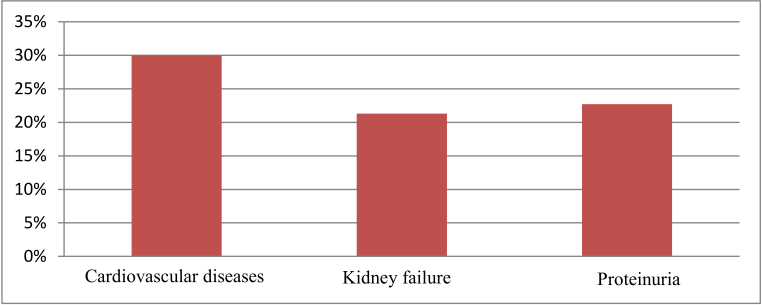
Chart 2. Characteristics of cardiovascular disease and other target organ damage of study sample
In our study, the rate of cardiovascular disease is 30%, the rate of kidney failure is 21.3% and the rate of proteinuria is 22.7%. Our results are much higher than the study of Vien Van Doan (2012) with the rate of myocardial infarction of 1.8%, renal failure 2.8%, proteinuria 9.8% [5]. However, our research is consistent with some literature around the world, according to Joshua A. Beckman et al., The incidence of cardiovascular disease in diabetic patients is 20%, according to ADA 2016, the rate of failure kidney in patients with diabetes is from 20-40% [8].
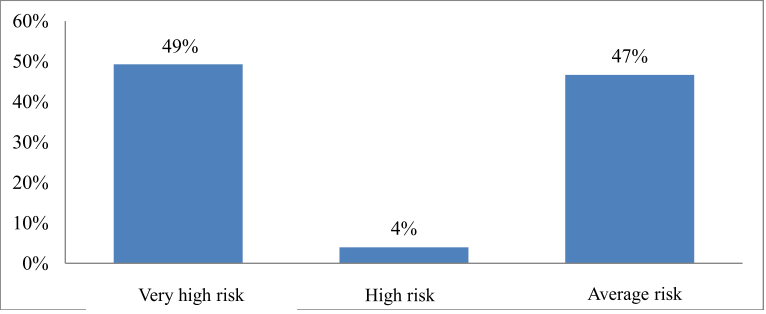
Chart 3. Stratification of cardiovascular risk factors among the research subjects
In our study, the very high risk group had the highest proportion at 49%, followed by the medium risk group with 47% and the lowest with the high risk group with 4%. In our opinion, the very high risk group accounts for a large proportion because the majority of patients after discovering cardiovascular disease (stroke, myocardial infarction …) or damage to the target organ (kidney failure …) has just been diagnosed with type 2 diabetes. This raises the issue of early screening for type 2 diabetes in the community for early treatment strategies and prevention of cardiovascular risk factors.
The average risk group also accounts for a relatively high proportion because the time to detect diabetes in the study sample is quite low, 95.3% is less than 10 years.
Table 1. Characteristics of several traditional cardiovascular risk factors in study sample
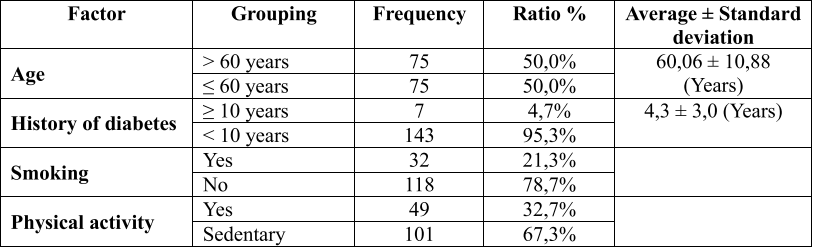
Associations of cardiovascular, hypertension and diabetes have long placed advanced age, duration of diabetes, smoking and physical activity into the group of cardiovascular risk factors. In our study, the rate of patients aged 60 and over is 50.0%, this result is relatively consistent with some other studies such as by Tran Thi Truc Linh (2016) with the rate of 60 years and over. to 68.1% [4] and Ina Maria Ruckert (2012) with this rate is 54.32% [13]. Up to 95.3% of patients have been diagnosed with diabetes for less than 10 years, this rate is higher than the study of Tran Thi Truc Linh (2016) with 78.4% [4]. The proportion of people having been diagnosed with diabetes for less than 10 years in our study is higher probably due to the poor awareness of screening, a not small part of detecting diabetes after being hospitalized for target organ damage. The rate of smoking and less physical activity in our study was 21.3% and 67.3%, this result is similar to many other studies such as Tran Thi Truc Linh (2016) when two billion This rate is 10.3% and 28.4 [4], the study of Leiter.Lawrence A (2013) smoking rate is 36.1% [11].
Table 2. Characteristics related to controlling BMI, waste circumference, arterial blood pressure according to ESC – EASD 2019
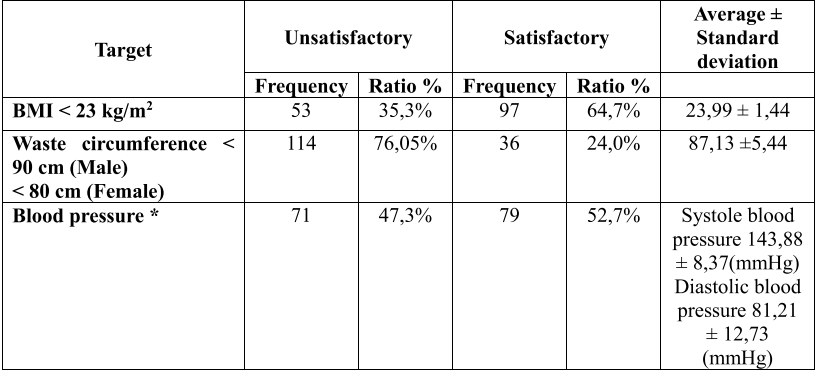
(* Individualization standards are outlined in the section “Standards used in research”)
In our study, the rate of BMI over 23 kg / m2 was 35.3% and the rate of increase in waist circumference was 76.05%. This result is similar to the study of Tran Thi An Nhan (2019) with a BMI of over 23 kg / m2 of 28.9% [3], the study of Tran Thi Truc Linh (2016) with a BMI of over 23 kg / m2 is 27.6% and the rate of increase in abdominal circumference is 64.7% [4]. It can be seen that abdominal fat has a much higher rate than being overweight, and we think a larger study is needed to find a link between increased waist circumference and type 2 diabetes.
In our study, the rate of uncontrolled blood pressure according to the goals of ESC – EASD 2019 is 47.3%, lower than that of Tran Thi Truc Linh (2016) with this rate of 59, 5% [4], this difference is due to the sample characteristics of the study above that patients with both type 2 diabetes and hypertension, and this study used a goal of controlling blood pressure according to the ESC – EASD 2013.
Table 3. Features of blood lipid control according to ESC – EASD 2019
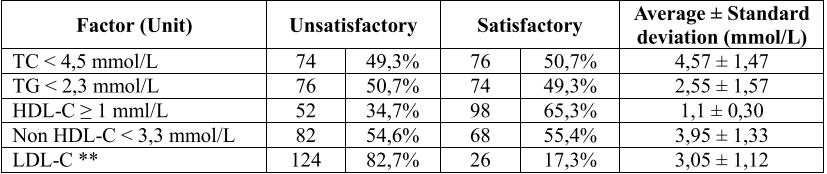
(** Individualization standards are listed under “Standards used in research”)
In our study, the rates of failure to meet the blood lipid control targets in diabetic patients according to ESC – EASD 2019 were: Total cholesterol 49.3%, Tryglicerid 50.7%, HDL-C 34, 7% and non HDL-C 54.6%. This result is quite similar to the study of Nguyen Le Phuong Anh (2019) with total cholesterol 52.1%, Tryglicerid 43.3% and Tran Thi Truc Linh’s study (2016) with total cholesterol 60.3%, Tryglicerid 40.5%, HDL-C 35.3% and non HDL-C 71.6% [2], [4]. As for LDL-C, after applying the individualized treatment goal according to cardiovascular risk stratification, the failure rate was quite high at 82.7%. This result is much higher than the study of Nguyen Le Phuong Anh (2019) with 46.0% and Tran Thi Truc Linh (2016) with 79.3% [2], [4]. This increase is because ESC – EASD 2019’s target of treatment recommendation in LDL-C control is more “rigorous” than ESC – EASD 2013, so the rate of LDL-C failure in our study quite tall.
Table 4. Features of blood glucose control according to ESC – EASD 2019
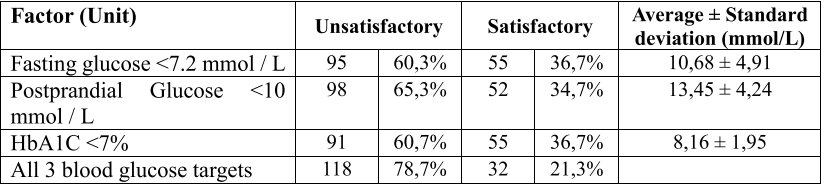
In our study, the group of patients did not reach the target of fasting glucose of 60.3%, postprandial glucose was 65.3%, HbA1c60.7%. The control group did not meet all three blood glucose targets with a relatively high rate of 78.7%.
The control of blood sugar in our study is somewhat better than the study of Tran Thi Truc Linh (2016) with the rate of not meeting the blood glucose targets are: fasting glucose 74.1%, postprandial glucose 77, 6%, HbA1c is 66.4%, all three target 90.5% blood glucose [4]. In our opinion, this is because our research team has a rather high rate of target organ damage, so patient compliance is somewhat more positive.
4. CONCLUSION
In our study:
- Characteristics of cardiovascular disease and target organ damage: cardiovascular disease rate is 30%, kidney failure rate is 3% and proteinuria rate is 22.7%.
- Stratification characteristics of cardiovascular risk factors: the very high risk group accounts for the highest proportion with 49%, followed by the medium risk group with 47% and the lowest is the high risk group with 4%
- Characteristics of some traditional cardiovascular risk factors: 50.0% of patients aged 60 years and older, 95.3% of patients with diabetes under 10 years, rate of smoking The leaves and less physical activity in our study were 21.3% and 3%.
- The target characteristics of controlling some cardiovascular risk factors in diabetic patients according to the guidance of ESC – EASD 2019: BMI rate above 23 kg / m2 is 35.3%, the rate of increase in abdominal circumference 76.05%, the rate of uncontrolled blood pressure was 3%.
- Characteristics of blood lipid control in diabetic patients as guided by ESC – EASD 2019: Total cholesterol 49.3%, Tryglicerid 50.7%, HDL-C 34.7% and non HDL-C 54 , 6% and LDL-C is 7%.
- Glucose control characteristics according to ESC – EASD 2019 guidelines: the percentage of patients who failed to reach the target of fasting glucose was 60.3%, after eating glucose was 65.3%, 7%.
REFERENCES
- Nguyen Hai Thuy, V. C. (2018). Diabetes, University Curriculum, Internal Medicine. Hue University Publishing House: Thua Thien Hue.
- Nguyen Le Phuong (2019). Survey on the situation of dyslipidemia in patients with type 2 diabetes at Hospital District 3 – HCMC Graduation thesis, Van Lang University.
- Tran Thi An Nhan. (2019). Ankle-arm blood pressure index and some related factors in type 2 diabetic patients at Central Highlands General Hospital in 2019. Grassroots-level scientific topic: University of the Central Highlands.
- Tran Thi Truc Linh. (2016). Study on the relationship between cardiac manifestations and targets according to ESC – EASD recommendation in hypertensive type 2 diabetic patients. Doctor of Medicine thesis: University of Medicine – Hue
- Vien Van (2012). Control Outcomes Some cardiovascular risk factors in diabetic patients that are managed and treated outpatiently at the Clinical Department, Bach Mai Hospital. . Bach Mai Hospital.
- WHO (2020). Viet Namstatistics summary (2002 – present). Global Health Observatory country views.
- Institute for Health Metrics and Evaluation (2017).Global Burden of Disease Study 2017. Global health data
- Beckman, A., Creager, M. A. & Libby, P. (2002). Diabetes and atherosclerosis: epidemiology, pathophysiology, and management. JAMA, 287(19), 2570-2581.
- Cosentino, , Grant, P. J., Aboyans, V., Bailey, C. J., Ceriello, A., Delgado, V., et al. (2020). 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J, 41(2), 255-323.
- Goyal, A., Gupta, , Singla, R., Kalra, S. & Tandon, N. (2020). American Diabetes Association “Standards of Medical Care- 2020 for Gestational Diabetes Mellitus”: A Critical Appraisal. Diabetes Ther.
- Halperin, I. J., Ivers, N. M. & Wong, (2013). Re: Leiter LA, Berard L, Bowering CK, et al. Type 2 Diabetes mellitus management in Canada: is it improving? Can J Diabetes 37;2:82-9. Can J Diabetes, 37(4), 213.
- Piepoli, M. , Hoes, A. W., Agewall, S., Albus, C., Brotons, C., Catapano, A. L., et al. (2016). 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J, 37(29), 2315-2381.
- Ruckert, I. M., Maier, , Mielck, A., Schipf, S., Volzke, H., Kluttig, A., et al. (2012). Personal attributes that influence the adequate management of hypertension and dyslipidemia in patients with type 2 diabetes. Results from the DIAB-CORE Cooperation. Cardiovasc Diabetol, 11, 120.
 Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam
Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam