CORRELATION BETWEEN SERUM Hs-CRP LEVELS WITH HbA1c AND INSULIN RESISTANCE IN TYPE 2 DIABETIC PATIENTS
Dao Thi Dua, Tran Huy Hoang, Nguyen Trong Nghia.
Hue Central Hospital.
ABSTRACT
Background:Diabetes is a disease of endocrine-metabolic properties with chronic hyperglycemia and cause many complications. Some studies have judged that the increase in concentration of hs-CRP serum is related to blood glucose control, insulin resistance. Objectives: 1. To determine the concentration of serum hs-CRP and the degree ofinsulin resistance in type 2 diabetic patients. 2. To survey the correlation between the concentration of serum hs-CRP and HbA1c and the Insulin resistance index in type 2 diabetic patients.Subiects and methods:50 patients diagnosed with type 2 diabetes according to American Diabetes Association in 2015, and 51 normal people as control group. Study design: cross-sectional study. Determine the amount of serum hs-CRP, fasting blood insulin, fasting blood glucose, HOMA-IR index = [Io (mU/L) x Go (mmol/L )] / 22.5, the index QUICKI = 1 / [Log I0 (μU / ml) + Log G0 (mg/dl)], McAuley index = Exp [2.63 to 0.28 ln I0 (μU/ml) – 0.31ln triglycerides (mmol/L)].Results:1. The concentration of serum hs-CRP in type 2 diabetic patients was 4.19 ± 1.55 mg/L and in control group was 1.49 ± 1.13 mg/L, The difference among them was significant (p <0.01). 2. Serum hs-CRP concentration was closely directly proportional correlation to HbA1c (r = 0.84; p <0.01). Serum Hs-CRP concentration was very closely directly proportional to HOMA-IR index (r = 0.59; p <0.01), to Io (r = 0.52; p <0.01), and very closely inversely proportional correlation,to McAuley index (r = -0.83; p <0.01), and to QUICKI index (r = -0.83; p <0.01). Multivariate recurrent equation: The concentration of serum hs-CRP = 10.245-.299 (McAuley) – 14.193 (QUICKI), and McAuley and QUICKI index independentely impacted on Serum hs-CRP concentration.Conclusions: 1. Hs-CRP concentration of serum in type 2 diabetic patients doubled these in the control group which had statistical significance. 2. There was correlation between hs-CRP concentration in serum and HbA1c and insulin resistance index in type 2 diabetic patients.
Main correspondence:Dao Thi Dua
Submission date: 9 Feb 2017
Revised date: 21 Feb 2017
Acceptance date: 15Mar 2017
1.BACKGROUND
Diabetes is an endocrin-metabolic disease with hyperglycemia nature and cause chronic complications affecting the quality of life significantly. Some studies in the country and around the world have identified several factors involved in inflammation in the pathology of diabetes, hs-CRP concentration in serum increases related to blood glucose control, insulin resistance. Stemming from the above issues we perform research: “Research correlation hs-CRP concentration in serum with HbA1c and insulin resistance in type 2 diabetic patients” with 2 goals : 1. To determine the concentration of serum hs-CRP and insulin resistance in type 2 diabetic patients. 2. To survey correlation between the concentration of serum hs-CRP and HbA1c and the Insulin resistance index in type 2 diabetic patients.
2. SUBJECTS AND METHODS
2.1. Study subjects:
The group of 50 type 2 diabetes patients treated at Hue Central Hospital, the control group of 51 normal subjects.
2.1.1. Patient selection criteria:
Patients had been diagnosed and treated for type 2 diabetes. New diagnosis of diabetes disease under the American Diabetes Association (ADA) 2015: 1 correspond to the following criteria: 1.HbA1c ≥6.5%. 2. Fasting Blood Glucose ≥7,0mmol / l (≥126mg / dl). 3. Blood glucose ≥ 11.1 mmol / l (200 mg / dl) at the time of 2 hours after the glucose tolerance test orally. 4. Have the symptoms of diabetes (clinical) and blood glucose at any time of ≥ 11.1 mmol / l (200 mg / dl).
2.1.2. Control selection criteria:
The usual, equivalent in age, gender, disease group, agreed to participate in the study.
2.1.3. Exclusion criteria:
The subjects with blood disorders: anemia, thalassemia …., liver disease or liver failure Park, the acute disease: infections, stroke, myocardial infarction … , malignancy, post-operative period, are using these drugs increase blood glucose: corticosteroids, thiazide diuretics, pregnant women.
2.2. Research Methods
2.2.1. Study design: cross-sectional study.
2.2.2. Research variables and how to proceed
– Age, gender
– Quantification of serum hs-CRP: by measuring the turbidity of Tina-spin.
Value for hs-CRP normal at about 0.8 mg/l – 8 mg/l.
– Quantification of fasting insulin immune method electrochemical luminescence. Since then calculate indirect indicators identified KI:
– HOMA-IR index = [Io (mU / L) x Go (mmol / L)] / 22.5. Restriction point: the highest quartile of the control group in our study was 2.00.
– Index QUICKI = 1 / [Log I0 (μU / ml) + Log G0 (mg / dl)]. Restriction point: choose the lowest quartile of the control group in our study was 0.34.
– Index McAuley = exp [2.63 to 0.28 ln I0 (μU / ml) – 0,31ln triglycerides (mmol / L)]. Restriction point: choose the lowest quartile of the control group in our study was 6.75.
2.2.3. Data processing: The rate is shown as a percentage (%) and tested by chi-square test chi-square χ2 determine average value, standard deviation SD, uses student t-test, test of Anova. To investigate the correlation between the parameters we calculated the correlation coefficient r with 95% confidence intervals. Risk assessment by odds ratio OR, with 95% CI does not include one.
3. RESULTS AND DISCUSSIONS
3.1. Characteristics of the study groups
Table 3.1. Distribution by age and gender
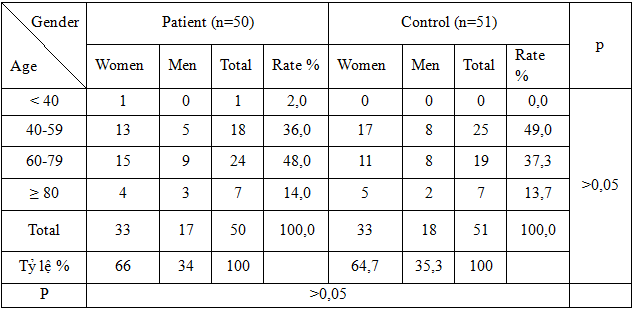 The distribution of patients by age, gender, as well as the distribution of sex ratios by age among type 2 diabetic patients and different control groups did not have statistical significance (p> 0.05).
The distribution of patients by age, gender, as well as the distribution of sex ratios by age among type 2 diabetic patients and different control groups did not have statistical significance (p> 0.05).
Table 3.2. The average value of a number of sub-clinical characteristics
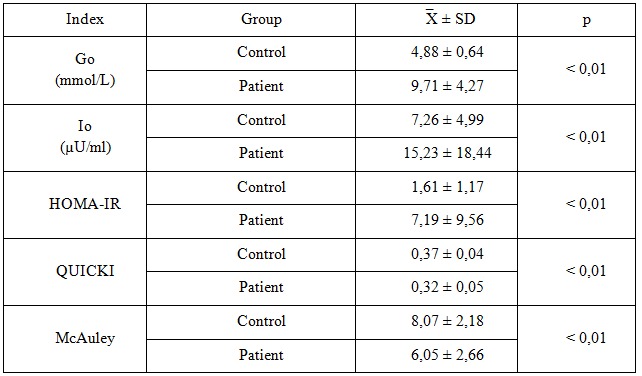 The concentration of Go, Io, Triglyceride, HOMA-IR index average patient group compared with the control group had a statistically significant p <0.01. QUICKI index, the index lower McAuley patient group compared with the control group was statistically significant with p <0.01. Cholesterol, HDL-C, LDL-C patients and control group difference was not statistically significant p> 0.05.
The concentration of Go, Io, Triglyceride, HOMA-IR index average patient group compared with the control group had a statistically significant p <0.01. QUICKI index, the index lower McAuley patient group compared with the control group was statistically significant with p <0.01. Cholesterol, HDL-C, LDL-C patients and control group difference was not statistically significant p> 0.05.
3.2. The concentration of serum hs-CRPand insulin resistance type 2 diabetic patients
3.2.1. The concentration of serum hs-CRP in patients with type 2 diabetes
Table 3.3. Hs-CRP concentration in serum group average type 2 diabetic patients
compared to control
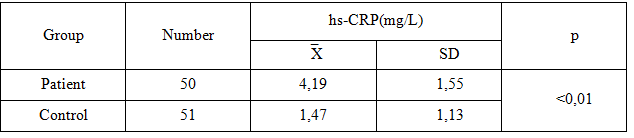 Hs-CRP concentrations of serum in type 2 diabetic patients was higher than the healthy group which had statisticalsignificance
Hs-CRP concentrations of serum in type 2 diabetic patients was higher than the healthy group which had statisticalsignificance
p <0.01.
Through the above results, it was found that the increase in the concentration of serum hs-CRP levels in type 2 diabetic patients was more centralized than the control group. Another point hs-CRP value was the average of the group of patients was still in the normal range, as usually when assessing the inflammatory lesions.
The result of our research was in line with the results of several other studies in the country and around the world such as:
Research by Le Thi Thu Huong performed on 89 type 2 diabetic patients and 38 healthy control results showed that hs-CRP levels of mean serum in type 2 diabetic patients was higher than the healthy group (5.15 ± 2.79 mg/L compared to 1.04 ± 1.27 mg / L; p <0.001) [12]. Bao Dung Vo study, Nguyen Hai Thuy also observed among patients with type 2 diabetes hs-CRP levels higher than the healthy group was statistically significant (3.60 ± 6.68 mg / ± 1.98 L versus 1.48 mg / L, p <0.001) [1].
A study by Fazlul Haque Haque A.K.M. and CS hs-CRP, concentration in serum in type 2 diabetic patients recorded concentrations of serum hs-CRP group’s average is 0.39 ± healthy person 0.24 mg/L and the group of patients with type diabetes 1.13 ± 1.58 mg 2/L. Hs-CRP concentrations of type 2 diabetes patients compared with the healthy group was statistically significant
(p <0.01) [7].
According to Nguyen Hai Thuy hs-CRP is considered a biological marker of cardiovascular ideal. Because it was a matter not only provided independent information on cardiovascular risk, but also easily measured by the test inexpensive and standardized with minor changes that did not require serum sample collection techniques or special probe. Also tested also many other advantages such as: test did not depend on food, had a prolonged half-life, there was a reference limit of kinetic significantly, can be measured easily and immunoassay standardized high sensitivity (detection of CRP concentrations <10 mg / L) provide similar results in the form of fresh serum, storage format, or as a frozen plasma, reflecting protein stability … [3].
According to our research hs-CRP levels of mean serum of patients with type 2 diabetes was 4.19 ± 1.55 mg / L, this value was quite high (hs-CRP> 3 mg/L) in cardiovascular risk stratification using hs-CRP levels as a factor to evaluate. This indicated that type 2 diabetic patients are more at risk of cardiovascular disease. Some studies: Pfutzner Andreas and CS, and CS Mahajan Anubha results showed that patients with type 2 diabetes have increased levels of hs-CRP, the risk of cardiovascular disease [8].
3.2.2. Insulin resistance in type 2 diabetic patients
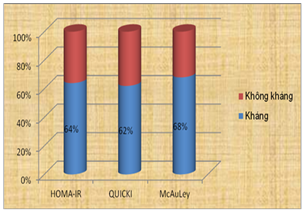
Figure 3.1. The distribution ratio of insulin resistance in type 2 diabetic patients
3.3. The correlation between the serum hs-CRP concentration with HbA1c and some insulin resistance index in type 2 diabetic patients.
3.3.1. The relationship and correlation between hs-CRP concentration in serum and HbA1c
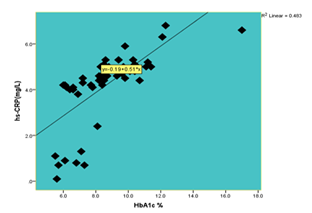
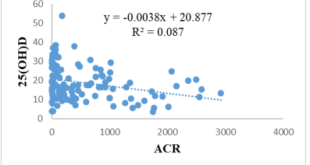
Figure 3.2. Correlation between hs-CRP index and HbA1c
Through our research results found that levels of serum hs-CRP closely correlated (r = 0.84; according to the equation: y = 0,51x – 0.19; p <0.01) with HbA1c.
The results of our study were similar to the results of several other studies, such as Andreas Pfutzner research and et al also showed that patients with higher HbA1c levels of serum hs-CRP as high [11]. Research by the authors Meshram Ajay, Udit Agrawal, Archana Dhok, Adole Prashant, Komal and Khare Ruchir Meshram also noted the strong correlation between hs-CRP concentrations and HbA1c [9]. Research by the authors Mahajan Anubha, Tabassum Rubina et al concluded that hs-CRP concentrations are markedly increased in both male and female genders in diabetic patients compared with healthy controls (P <0.0001). The increase in the concentration of serum hs-CRP had a positive correlation with type 2 diabetes (OR = 1.66; P <0.002), even after adjusting for factors of obesity [8]. Research by the authors Mohamed Abdelrahman Mohamed Salih, Mustafa Elfaki Elyasa, Yassir Basher Basher and Fadul noted hs-CRP levels in serum of patients group (2.69 ± 3.10 mg/L) obviously higher than the control group ( 0:47 ± 0:12 mg / L) p = 0.000; hs-CRP concentration in serum in people with hypertension compared with those without hypertension (7:03 ± 1.62 mg/L) compared to 1.65 ± 1:06 mg/L; p = 0.000). Hs-CRP concentrations in type 2 diabetic patients are also higher female gender than male (3.65 ± 2.92mg/L compared to 2:53 ± 2:34 mg/L; p = 0.037). Also the results also showed a strong correlation between hs-CRP levels in serum blood glucose starvation (r = 0.91, p = 0.000); HbA1c (r = 0.88, p = 0.000); BMI (0.91, p = 0.000) and total cholesterol (r = 0.78, p = 0.000) [10]. In the study by Gohel Anusha Mukesh G. and N. Chacko over 150 people were divided into 3 groups: group 1 included 50 healthy people, group 2 is 50 type 2 diabetic patients have blood glucose control is good and the group 3 of 50 people with poor blood glucose control levels. The study results showed that levels of serum hs-CRP in group 3 had higher values than group 1 and group 2 and group 2 than group 1 (p <0.001). Moreover there is a very clear correlation between the concentration of serum hs-CRP with HbA1c [6]. The studies were recorded concentrations of serum hs-CRP closely correlated with HbA1c.
3.3.2. The correlation between serum concentration with some insulin resistance index in type 2 diabetic patients.
Table 3.4. Correlation between Hs-CRP levels with insulin resistance index
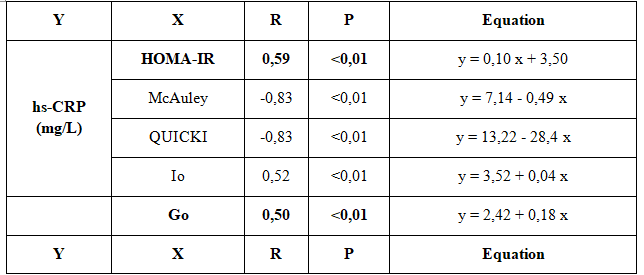 Table 3.5. Correlation multivariate regression hs-CRP concentrations
Table 3.5. Correlation multivariate regression hs-CRP concentrations
with indicators of insulin resistance
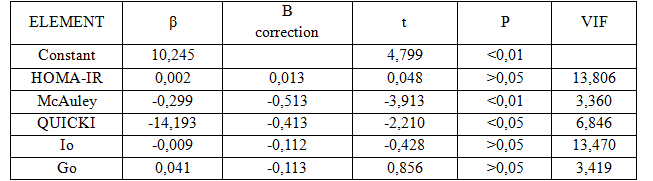 The results of our research recognized that hs-CRP concentrations were correlated with other indicators to evaluate the status KI: there was very close correlation with HOMA-IR index (r = 0.59; p <0.01, according to the equation: y = 0.1x + 3.5). There was a very strong negative correlation with the index McAuley index (r = -0.83; p <0.01; under the works: y = 7,14 – 0,49x). There was a very strong negative correlation with QUICKI index (r = -0.83; p <0.01; according to the equation: y = 13.22 to 28, 4x). There is a very tight positive correlation with Io (r = 0.52; p <0.01; according to the equation: y = 3.52 + 0,04x). Multivariate regression: hs-CRP concentration in serum = 10.245-.299 (McAuley) – 14.193 (QUICKI). We saw indicators and McAuley QUICKI independent influence hs-CRP concentrations to serum have statistical significance.
The results of our research recognized that hs-CRP concentrations were correlated with other indicators to evaluate the status KI: there was very close correlation with HOMA-IR index (r = 0.59; p <0.01, according to the equation: y = 0.1x + 3.5). There was a very strong negative correlation with the index McAuley index (r = -0.83; p <0.01; under the works: y = 7,14 – 0,49x). There was a very strong negative correlation with QUICKI index (r = -0.83; p <0.01; according to the equation: y = 13.22 to 28, 4x). There is a very tight positive correlation with Io (r = 0.52; p <0.01; according to the equation: y = 3.52 + 0,04x). Multivariate regression: hs-CRP concentration in serum = 10.245-.299 (McAuley) – 14.193 (QUICKI). We saw indicators and McAuley QUICKI independent influence hs-CRP concentrations to serum have statistical significance.
According to research by the authors Preethi BL, KM Prasanna Kumar, Suresh KP Jaisri .G and, along with the increase in the index to evaluate the status KI is the increase of hs-CRP concentration in serum and the like hs-CRP concentration in serum may have a role in the early exploration KI status in healthy people [12]. Research by the authors Mahajan Anubha, Rubina Tabassum, Chavali Sreenivas, Om Prakash Dwivedi, Bharadwaj Mausumi, Nikhil Tandon and Dwaipayan Bharadwaj also recorded along with the rise of the index, such as BMI, HOMA-IR, VB measurements. .. in the group of patients with type 2 diabetes is increased hs-CRP concentrations [8]. Bizu Gelaye Research and colleagues (2010) in 1525 subjects showed increased hs-CRP concentration in serum has a positive correlation with the increase in insulin levels of hunger and HOMA-IR index (p <0.001 [5]. the study’s authors Marzieh Akbarzadeh, Hassan and Hossein Mohammad Mohammad Eftekhari also noted a positive association between hs-CRP levels and indicators to evaluate the status KI [4].
The study showed close correlation between the CRP concentration in serum and hs-KI situation.
4. RESULTS
4.1. The concentration of serum hs-CRP in type 2 diabetic patients was 4.19 ± 1.55 mg/L and in control group was 1.49 ± 1.13 mg/L, The difference among
4.2. Serum Hs-CRP concentration was closely directly proportional to HbA1c (r = 0.84; p <0.01). Serum hs-CRP concentration was very closely directly proportional to HOMA-IR index (r = 0.59; p <0.01), to Io (r = 0.52; p <0.01), and very closely inversly proportional to McAuley index (r = -0.83; p <0.01), to QUICKI index (r = -0.83; p <0.01). Multivariate recurrent equation: The concentration of serum Hs-CRP = 10.245-.299 (McAuley) – 14.193 (QUICKI), and McAuley and QUICKI index indepentely impacted on serum hs-CRP concentration.
5. CONCLUSION
5.1. Hs-CRP concentration of serum in type 2 diabetic patients doubled that of the control group which had statistical significance.
5.2. There was correlation between hs-CRP concentration in serum and HbA1c and insulin resistance index in type 2 diabetic patients.
REFERENCES
- Võ Bảo Dũng, Nguyễn Hải Thủy, Hoàng Minh Lợi (2012), “Liên quan giữa đáp ứng giãn mạch qua trung gian dòng chảy với hs-CRP và đề kháng insulin ở bệnh nhân đái tháo đường týp 2 mới phát hiện”, Tạp chí nội tiết đái tháo đường kỷ yếu toàn văn các đề tài khoa học hội nghị nội tiết và đái tháo đường toàn quốc lần thứ VI. 2(7), tr. 699-705.
- Lê Thị Thu Hương (2012), “Liên quan giữa nồng độ protein phản ứng C huyết thanh độ nhạy cao với một số yếu tố nguy cơ tim mạch lâm sàng ở bệnh nhân đái tháo đường type 2”, Tạp chí nội tiết đái tháo đường kỷ yếu toàn văn các đề tài khoa học hội nghị nội tiết và đái tháo đường toàn quốc lần thứ VI. 2(7), tr. 543-554.
- Nguyễn Hải Thủy (2012), “Vai trò chất chỉ điểm sinh học trong bệnh lý xơ vữa động mạch”, Tạp chí nội tiết đái tháo đường kỷ yếu toàn văn các đề tài khoa học hội nghị nội tiết và đái tháo đường toàn quốc lần thứ VI. 2(7), tr. 255-269.
- Akbarzadeh Marzieh, Eftekhari Mohammad Hassan, Dabbaghmanesh Hossein Mohammad et al (2013), “Serum IL-18 and hsCRP correlate with insulin resistance without effect of calcitriol treatment on type 2 diabetes”, Iranian Journal of Immunology. 10(3), pp. 167-176.
- Gelaye Bizu, Revilla Luis, Lopez Tania et al (2010), “Association between insulin resistance and c-reactive protein among Peruvian adults”, Gelaye et al. Diabetology & Metabolic Syndrome. 2(30), pp. 1-6.
- Gohel Mukesh G., Chacko Anusha N. (2013), “Serum GGT activity and hsCRP level in patients with type 2 diabetes mellitus with good and poor glycemic control: an evidence linking oxidative stress, inflammation and glycemic control”, Journal of diabetes and metabolic disorders. 12(1), pp. 56.
- Haque Fazlul A.K.M., Saifuddin Ekram A.R.M., Islam Quazi Tarikul et al (2010), “Evaluation of serum high sensitivity c – reactive protein (hs-CRP) in type-2 diabetic patient”, J Medicine. 11(1), pp. 20-23.
- Mahajan Anubha, Tabassum Rubina, Chavali Sreenivas et al (2009), “High-sensitivity C-reactive protein levels and type 2 diabetes in urban North Indians”, Journal of Clinical Endocrinology and Metabolism. 94(6), pp. 2123-2127.
- Meshram Ajay, Agrawal Udit, Dhok Archana et al (2013), “HbA1c, hs-CRP and anthropometric parameters evaluation in the patients of diabetes mellitus of Central Rural India”, Int J Med Sci Public Health. 2(2), pp. 293-296.
- Mohamed Abdelrahman, Mohamed Salih, Mustafa Elfaki Elyasa et al (2012), “Assessment of plasma levels of high sensitive c – reactive protein and cholesterol among Sudanese with type 2 diabetes mellitus”, J.Sc. Tech. 12(3), pp. 29-35.
- Pfützner Andreas, Standl Eberhard, Strotmann Hermann-josef et al (2006), “Association of high-sensitive C-reactive protein with advanced stage beta-cell dysfunction and insulin resistance in patients with type 2 diabetes mellitus”, Clinical chemistry and laboratory medicine 44(5), pp. 556-560.
- Preethi B.L., Prasanna Kumar K.M., Jaisri G et al (2013), “High-sensitivity C-reactive protein a surrogate marker of insulin resistance”, Journal of Physiology and Pathophysiology. 4(3), pp. 29-36.
 Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam
Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam