EVALUATION OF ANTHROPOMETRIC INDICES IN NEWLY-DIAGNOSED PREDIABETES IN QUANG BINH PROVINCE
Le Viet Hung, Nguyen Hai Thuy*, Tran Huu Dang*,
Nguyen Hai Ngoc Minh**, Le Thi Hue
Quang Binh Medical College, * Hue University of Medicin and Pharmacy,
** Da Nang Family Hospital
DOI: 10.47122/vjde.2022.53.9
ABSTRACT
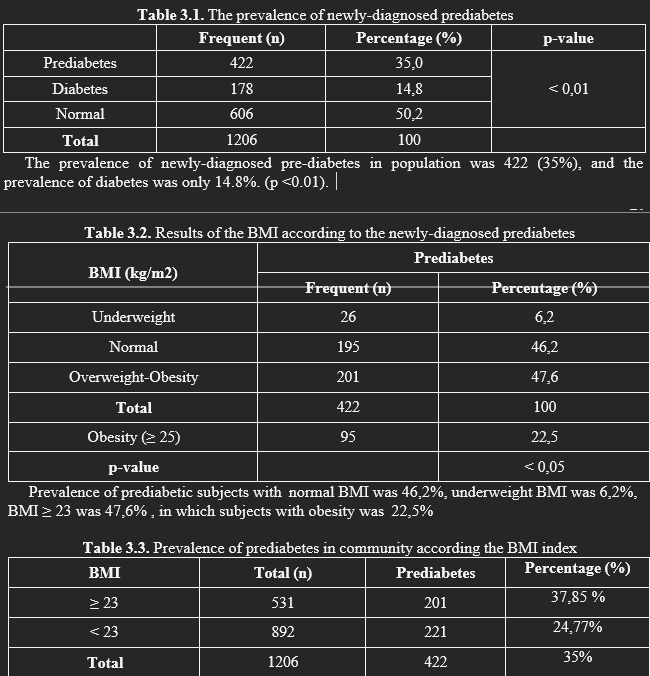
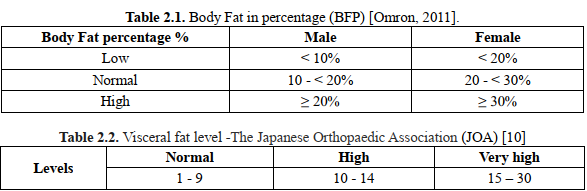
Pre-diabetes is a term that describes a condition in which a person has higher than normal glucose levels but does not meet the criteria for a diagnosis of diabetes. Clinically, obesity is assessed through anthropometric indices such as BMI, waist circumference (WC), body fat percentage (BFP), and visceral fat (VPF). Objectives: 1. Determine the rate of newly diagnosed pre-diabetic subjects in the community in Quang Binh province; 2. Evaluate of anthropometric indicators in newly diagnosed pre-diabetic subjects. Methods: A descriptive cross-sectional study was conducted on 1206 non-diabetic and pre-diabetic adults (ages range from 20 to 60 years) from Quang Binh province. Results: Prevalence of prediabetic subjects with normal BMI was 46,2%, underweight BMI was 6,2%, BMI ≥ 23 was 47,6% , in which subjects with obesity was 22,5% .The mean waist circumference in pre-diabetic men with central obesity was 81,71
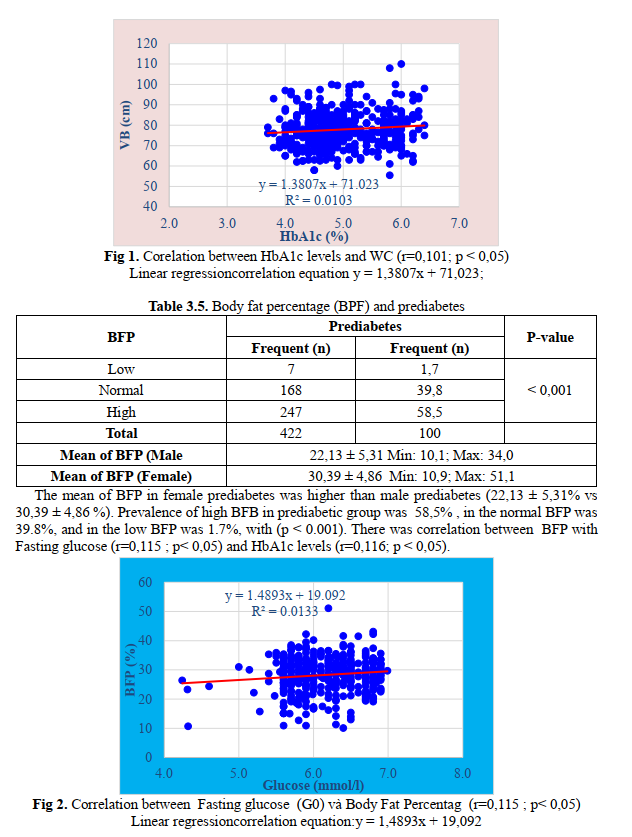
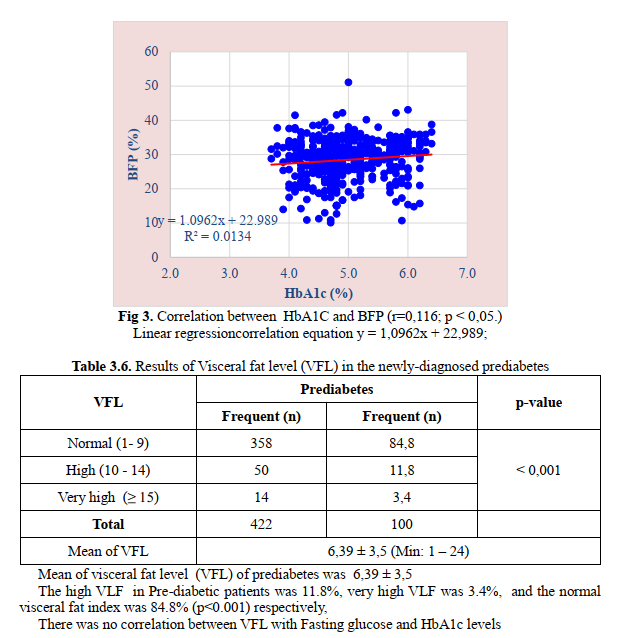
± 8,08 cm and in pre-diabetic women, the average waist circumference was 76,79 ± 8,48 cm. Prevalence of central obesity in Pre- diabetes group was found 31.3% and 68.7% of people without central obesity (p < 0,05). There was a correlation between HbA1c levels and WC (r=0,101; p < 0,05).The mean of BFP in female prediabetes was higher than male prediabetes (22,13 ± 5,31% vs 30,39 ± 4,86 %) .Prevalence of high BFB in prediabetic group was 58,5% , in the normal BFP was 39.8%, and in the low BFP was 1.7%, with (p < 0.001).There was correlation between BFP with Fasting glucose (r=0,115 ; p< 0,05) and HbA1c (r=0,116; p < 0,05).Mean of visceral fat level (VFL) of prediabetes was 6,39 ± 3,5 .The high VLF in Pre-diabetic patients was 11.8%, very high VLF was 3.4%, and the normal visceral fat index was 84.8% (p<0.001).respectively, There was no correlation between VFL with Fasting glucose and HbA1c levels. Conclusions: Clinical Usefulness of Waist circumference and body fat percentage (Anthropometric Indices) to Predict the Presence of Prediabetes in Central Vietnam.
Key words: adiposity, body composition, prediabetes, HbA1C, obesity
Main correspondence: Le Viet Hung
Submission date: 1th Dec 2022
Revised date: 15th Dec 2022
Acceptance date: 30th Dec 2022
Email: [email protected]
1. INTRODUCTION
Pre-diabetes is a term that describes a condition in which a person has higher than normal glucose levels but does not meet the criteria for a diagnosis of diabetes.. Prediabetes is also associated with an accumulation of metabolic abnormalities, an increased risk of microangiopathy and cardiovascular disease. Obesity was clinically assessed using anthropometric indices such as BMI, waist circumference (WC), body fat percentage (BFP), and visceral fat (VFL).
According to the Health Ministry of Vietnam’s recent figures, the rate of diabetes in the 30-69 age group would be 5.8%, whereas the rate of impaired fasting glucose (IFG) (pre- diabetes) is 3.6% and tends to be youthful. Only 31.1% of diabetes patients are diagnosed, as well as the majority are admitted to the hospital at a late stage. Diabetes cases with hyperglycemia were managed in healthcare presets 28.9% of the time [MOH, 2015].
Therefore, so, this long asymptomatic stage needs more attention, and the detection of prediabetes in patients with a high metabolic risk should be considered. One way to test this screening may be by assessing body composition, the anthropometric indices in newly-diagnosed prediabetes.
2. METHODS
2.1 Subjects: We recruited non- diabetic/pre-diabetic adults (ages range from 20 – 60 years) from Quang Binh province. The study was conducted from July 2021 to August 2022 (15 months).
2.2 Study design: cross sectional, descriptive. The sample size was calculated using the formula. The number of sample size was about 1200 participants.
2.3 Diagnotic Criteria: According to the Guidelines for diagnosis and treatment of diabetes by the Ministry of Health issued (July 16, 2020) and the American Diabetes Association-ADA 2021: Prediabetes was defined as HbA1c 5.7–6.4% (39–46 mmol/mol), impaired fasting glucose (IFG) (FPG=6.1–6.9 mmol/L).
Asia Pacific Criteria by Alberti et al has categorized waist circumference as normal and abnormal; also identified that WC cut-offs of ≥ 90 cm in men and ≥ 80 cm in women have high odds ratio for cardiovascular risk factors[Alberti 2005].
BMI was further categorized as per Asia Pacific guidelines into lean to normal (≤22.9), overweight (23–24.9) and obese groups (≥25) (WHO 2005).
2.4. Statistical analysis
The data are reported as mean, standard deviation, absolute number, and percentage. The statistical analysis was carried out using the chi-square test. A value of p < 0.05 was considered significant. All the data were run on SPSS software (IBM SPSS Statistics for Windows, Version 23.0.).
3. RESULTS
We conducted a randomized study on 1206 subjects aged 20-60 years old in Quang Binh province from July 2021 to September 2022.
In a community of 1206 people, the prevalence of prediabetes in BMI ≥ 23 group was higher than in the BMI < 23 group (37.85% vs 24.77%, p < 0.05).
There was not a correlation between BMI with HbA1c levels and FG
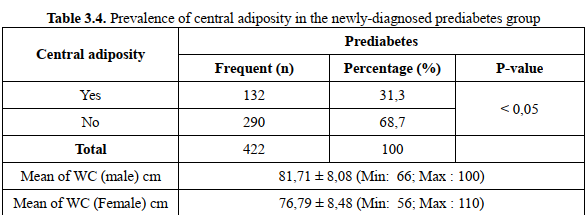
The mean waist circumference in pre-diabetic men with central obesity was 81,71 ± 8,08 cm and in pre-diabetic women, the average waist circumference was 76,79 ± 8,48 cm.
Prevalence of central obesity in Pre-diabetes group was found 31.3% and 68.7% of people without central obesity (p < 0,05).
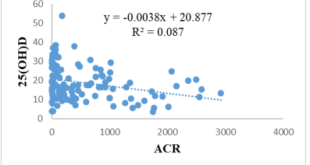
There was a correlation between HbA1c levels and WC (r=0,101; p < 0,05) but not with fasting glucose.
4. DISCUSSION
4.1. Overweight and prediabetes
Insulin resistance is fundamental in the pathogenesis of diabetes, so for a long time, BMI, an indicator of overweight and obesity, has been considered a risk factor for the disease.
In our study, the prevalence of diabetes with an overweight-obesity BMI (BMI ≥ 23) was 47.6% higher than that of the group with a normal BMI.
At the same time, in the population of 1206 subjects, the prevalence of pre-diabetes in the BMI ≥ 23 group was also higher than in the BMI < 23 group (37.85% versus 24.77%, p < 0.05).
This result is similar to the results of previous studies of June M. Chan and CS, who followed more than 50,000 people, found that a BMI ≥ 25 kg/m2 significantly increased the risk of diabetes compared with the BMI < 23 kg/m2 group [33]. Michael L. Ganz performed a case-control study of more than 37,000 people and noted that BMI is a very important risk factor for type 2 diabetes and that this risk increases as BMI increases from overweight to obese. 1, 2, and 3 were the highest risks for diabetes [Ganz, 2014].
Abtahi also noted that the higher the BMI, the higher the prevalence of diabetes and DM [6].
However, if we use the common Western countries’ criteria for diagnosing overweight and obesity (25 kg/m2 and > 30 kg/m2), the results show that the obesity rate in Asian countries is lower than that in Western countries.
Asians, especially South Asians, tend to have more central obesity and be more insulin resistant than people in Western countries.
Therefore, waist circumference (reflecting central abdominal obesity) is more strongly associated with diabetes than BMI.
Therefore, waist circumference (reflecting central abdominal obesity) is more strongly associated with diabetes than BMI.
Because of the numerous factors mentioned above, WHO reviewed the diagnostic criteria for obesity in Asians in 2000 and introduced a new criterion, according to which overweight was diagnosed when BMI was ≥ 23 kg/m2, obesity was diagnosed when BMI was ≥ and obesity was diagnosed when BMI was ≥ 27.5 kg/m2 [9].
Pham Thi Hong Phuong et al. (2012) studied some risk factors for prediabetes and diabetes in Quang Ngai province with ages ranging from 30 to 69; the prevalence of diabetes was 20.3% higher in subjects with a BMI≥23 than in subjects with a low BMI[3].
Chi Pang Wen studied the increase in risk factors for pre-diabetes in Taiwan with 36,386 people aged 40–49, who showed that BMI gradually increased with fasting glycemic index.
If blood sugar is < 5.6 mmol/l, BMI is 22.3; if glucose is between 5.6 – 6.1 mmol/l,
BMI is 23.2, glucose is between 6.1 – 6.9 mmol/l, BMI is 24.3; if glucose is >7 mmol/l, BMI is 24.6 [8].
As can be seen, the majority of the studies sample high-risk, elderly subjects, so the rate of IFG in these subjects is higher than in the normal control group.
As demonstrated in the preceding research reports, BMI is a critical risk factor in determining the risk of pre-diabetes and diabetes. However, there was no correlation between BMI with fasting blood glucose and HbA1c level in the study.
4.2. Central obesity and prediabetes
Obesity is found to be linked to not only chronic diseases such as diabetes, cardiovascular disease, hypertension. There have been many experimental studies showing that complications of obesity, such as diabetes, are the result of abnormal metabolism, an excess of free fatty acids, and triglycerides in non-adipose cells.
Studies have also demonstrated that when the beta cells of the pancreas are overloaded with fat, they become adipose-toxic, which causes cell death.
This is also an argument to explain the progressive, decades-long progression of the preclinical stage in people with type 2 diabetes. Obesity rates are increasing in Asia- Pacific countries, where economies are growing strongly.
In Vietnam, the prevalence of obesity is increasing among people in big cities. To assess obesity, people often use waist circumference (WC) and body mass index (BMI). BMI is an indirect measure of body fat, while waist circumference (WC) is used to assess obesity (abdomen). Central obesity has been implicated as a trigger for insulin resistance.
According to our findings, the rate of diabetes with male obesity was 31.3%, compared to 68.7% without male obesity (p<0.05). The mean waist circumference in men with diabetes was 81.71 ± 8.08 (cm) and the mean circumference in women with pre- diabetes was 76.79 ± 8.48 cm.
The findings of our study revealed that the pre-diabetic group with WC at risk accounted for a lower proportion when compared to research conducted by national and international authors.
Nguyen Kim Hung et al (2004) found that the rate of IFG in subjects with large WC was higher than in subjects with normal WC, 18.1% vs. 6.9%, (p < 0.001).
Le Anh Tuan (2010) recorded that the proportion of central obese with IFG was higher than that of those without it: 24.5% compared with 10%, (p<0.01).
The mean waist circumference in the study of the prediabetes Le Anh Tuan was 87.4 ± 8.7 (male) and 84.6 ± 8.6 (female), (p<0.01). Nguyen Thi Kim Cuc, Tran Huu Dang also recorded that the male obesity rate accounted for 69.7% (males accounted for 36.8%, females accounted for 83.3%) in
people with prediabetes [1] [4].
Yuan Song et al. (2019) screened 3,144 people in Bengu City, China, up to 40.5% of people with diabetes had central adiposity, and 20.5% did not have a large waist circumference; the average waist circumference of pre-diabetic subjects was 86.6 ± 10.9 cm (p<0.001).
Our study showed that waist circumference was not correlated with fasting blood glucose concentration but correlated with HbA1c (r = 0.101; p < 0.05) with the linear regression correlation equation y = 1.3807x + 71,023.
Our study showed that waist circumference was not correlated with fasting blood glucose concentration but correlated with HbA1c levels (r = 0.101; p < 0.05) with the linear regression correlation equation: y = 1.3807x + 71,023.
4.3. Body fat percentage (BFP) with prediabetes
Adipose tissue not only stores energy, but it also stores triglycerides in the body. Scientists have learned that measuring body fat percentage directly as a health expenditure will replace BMI as it is more accurate in assessing obesity now that technology has advanced. Body fat percentage (BFP) rather than body mass index (BMI) predicts risks for diseases related to body weight [5].
Through our study, the prediabetes rate in the group with a high body fat percentage accounted for 58.5%, the group with a normal body fat percentage accounted for 39.8%, and the group with a high body fat percentage accounted for the majority. Low body fat accounted for only 1.7% (p < 0.001).
Nguyen Kim Hung et al. found that people with a high percentage of body fat have a 2.5 times higher risk of DR than people with a normal body fat percentage, which is also consistent with the study in Hue City by the author Ho. Thi Thuy Vuong et al. (2009) showed that the rate of T2D in the group with a high body fat percentage of 10.5% and 6.2% was much higher than in the group with a normal percentage of body fat (2.4% and 0.9%).
The pre-diabetic group has a high percentage of body fat, accounting for 85.9% [5].In our study, there was a correlation between body fat percentage (BFP) and fasting blood glucose concentration (G0) (r=0.115; p<0.05) with the linear regression correlation equation: y = 1.4893x + 19,092; and also with HbA1c concentration (r=0.116; p < 0.05) with the linear regression correlation equation: y = 1.0962x + 22,989;
4.4. Visceral fat level (VFL) with prediabetes
Recent study, inactive participants had an 8.6% increase in VFL after 8 months, while physically active participants had an 8.1% decrease in VFL. According to the report of the Japan Obesity Association’s (JOA) Committee to Examine the Diagnostic Criteria for Obesity, the associated disease complications such as hypertension, diabetes, and cardiovascular disease have increased by more than 1.5 times if the VFL area > 100 cm. Disease complications double when the VFL area exceeds 150 cm [5].
In our study, the rate of pre-diabetes with high and very high visceral fat index was 15.2%, while the rate of pre-diabetes with normal visceral fat index was 84.8%, a statistically significant difference (p<0.001).
A study in Hue City by HTV et al. (2009) showed that the pre-diabetic group had 65.4% of people with a high VFL percentage, and the diabetic group had 67.4% of people with high visceral fat [5].
According to the study by Shuying Li et al. (2022), adults with pre-diabetes or diabetes had a higher visceral fat index, body fat percentage, WC, and BMI than those with a normal glucse level.
There is a positive correlation between HbA1c and fasting blood glucose in pre- diabetics and the general population, with indicators related to obesity.
There may be a tendency toward fat loss in type 2 diabetes with poor glycemic control (HbA1c > 7%). Independent of BMI, the visceral fat index (VFL) may have an adverse effect on glucose metabolism. WC is ideal for determining the risk of impaired glucose metabolism [Li S, 2022].
According to Tram N.H.Q (2011), men and women with high levels of visceral fat (VFL) are more likely to have hypertension, hyperglycemia, and high cholesterol than those with a BMI of 23.
Thus, there is a link between body fat, visceral fat, and hyperglycemia.
People with a high percentage of body fat and a high visceral fat index are more likely to have prediabetes or diabetes, and people with prediabetes or diabetes often have a high body fat to visceral fat ratio.
As a result, data on body fat and visceral fat percentage should be collected in community screening for prediabetes. However, we found no correlation between the visceral fat and fasting glucose or HbA1c [2].
CONCLUSIONS
Through a study of 1206 subjects aged 20– 60 in Quang Binh province, we recorded that there were 422 newly diagnosed pre-diabetes, accounting for 35% (422/1206), including 76.8% female participants and 23.2% male
participants (23.2%).
Pre-diabetic subjects with a BMI ≥ 23 comprised 47.6% of the total . In a community survey, the prevalence of prediabetes in the BMI ≥ 23 group was higher than in the BMI
<23 group.(37,85% versus 24.77%, p <0.05). but there are no correlation between BMI with fasting glucose or HbA1c levels.
Subjects with prediabetes with waist circumference risk of 31.3% and there was a correlation between WC and the HbA1c levels (r = 0.101, p = 0.038).
The pre-diabetic group had a high body fat percentage (BFP) of 58.5%. In both sexes, there are relationship between the indices (BFP) with fasting glucose ( r = 0.115 and p<0.024) and HbA1c levels (r = 0.16, p = 0.017).
The pre-diabetic group had a high level of visceral fat (VFL) of 15.2% but there are no correlation between VFL with fasting glucose or HbA1c levels.
Clinical Usefulness of Waist circumference and body fat percentage (Anthropometric Indices) to Predict the Presence of Prediabetes in Central Vietnam.
REFERENCES
1. Nguyễn Kim Cúc, Trần Hữu Dàng (2011), Nghiên cứu các yếu tố nguy cơ gây nên tiền đái tháo đường của người dân trong độ tuổi lao động tại thành phố Đà Nẵng năm 2009, Tạp chí Nội tiết – Đái tháo đường, (2), tr.175-83.
2. Nguyễn Hải Quý Trâm và Hoàng Khánh Hằng (2011), “So sánh giá trị tỷ lệ mỡ cơ thể (BFP), mức mỡ nội tạng (VFL) với BMI, vòng bụng và một số yếu tố nguy cơ tim mạch-chuyển hoá”, Tạp chí Y Dược học- Trường ĐH Y Dược Huế, số 2/2011, tr.131
3. Phạm Hồng Phương, Lê Quang Toà và cộng sự (2012), “Khảo sát một số yếu tố nguy cơ liên quan đến bệnh đái tháo đường týp 2 và tiền đái tháo đường tại tỉnh Quảng Ngãi”, Kỷ yếu Hội nghị Nội tiết-Đái tháo đường toàn quốc lần VIII, số 8, tr.95-105.
4. Lê Anh Tuấn và Nguyễn Hải Thuỷ (2010), “Rối loạn dung nạp glucose ở người trên 45 tuổi đến khám tại bệnh viện quận Hải Châu thành phố Đà Nẵng”, Y học thực hành, số 718+719, 135-144.
5. Vương Hồ Thị Thuỳ, Nguyễn Hải Thuỷ (2009), “Nghiên cứu tỷ lệ mỡ cơ thể (BFP) và mức mỡ nội tạng (VFL) trong giai đoạn tiền đái tháo đường”, Tạp chí Nội khoa, Kỷ yếu toàn văn các đề tài khoa học đại hội và hội nghị nội khoa toàn quốc lần thứ VI, số 1/2009, tr. 444-453.
6. Abtahi, A. N. F, Zibaeenezhad MJ, Heydari S.T., et al (2010), “The Relationship between Body Mass Index and Pre-Diabetes In Teachers Residing in Shiraz-Iran 2009”. Iranian Cardiovascular Research Journal, 4(3), 112-117.
7. Chan, J. M., Rimm, E. B., Colditz, G. A., Stampfer, M. J., Willett, W. C. (1994), “Obesity, fat distribution, and weight gain as risk factors for clinical diabetes in men”. Diabetes Care, 17(9), 961-969.
8. Wen, C. P., Cheng, T. Y. D., Tsai, S. P., et al (2005). Increased Mortality Risks of Pre- Diabetes (Impaired Fasting Glucose) in Taiwan. Diabetes Care, 28 (11), 2756–2761.
9. WHO expert consultation (2004), “Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies”. Lancet, 363(9403), 157-163.
10. Zhao, D., Wu, N., Yang, J., Liu, S., et al. (2015), “The Prevalence and Associated Risk Factors of Impaired Glucose Regulation in Chinese Adults: A Population-Based Cross-Sectional Study”.International Journal of Endocrinology,2015, 731583.
 Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam
Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam