INVESTIGATION OF PLASMA LEPTINLEVER IN PATIENTS WITH
TYPE 2 DIABETES MELLITUS
Nguyen Van Hoan1,2, Nguyen Thanh Binh2, Nguyen Linh Toan3§
1Department of Endocrine, 103 Military Hospital,
Vietnam Military Medical University, Ha Dong, Hanoi, Vietnam
2Nghe An Endocrine Hospital, Nghe An,Vietnam
3 Department of Pathophysiology,Vietnam Military Medical
University, Ha Dong, Hanoi, Vietnam
Corresponding author:
ABSTRACT
Aim: Adipose tissue-derived hormones are associated with metabolic disorders including T2DM.This study investigatedclinical parameters and the levels ofleptin cytokineinpatients withtype 2 diabetes mellitus (T2DM) patients with or without overweight/obese. Materials and Methods: Based on body mass index (BMI), 130 patients with T2DM were divided either as overweight/obese or non-overweight/non-obese subjects. 125overweight/obese and non-overweight/non-obese individuals devoid of T2DM were included as healthy controls. The leptinlevelswere measured in the plasmasamples in all study subjects byELISA and clinical parameters. Results: The leptin levelswere significantly lower in patients withT2DM [median: 1202.75 pg/ml] compared to controls[median: 1715.4 pg/ml] (P=0.05). Theleptinlevels were increased in overweight/obese T2DM patients and inoverweight/obese healthy subjects compared to without overweight/obese T2DM patients and healthy induviduals (p<0.05). The levels of leptin were significantly increased in female patients with T2DM and in T2DM patients with metabolic syndrome (MS) compared to those of male patients (P<0.001) and T2DM patients with none-MS (P<0.05). Conclusions: Leptin cytokineis associated with T2DM andmay serve as a prognostic marker for overweight/obese-related T2DM.
Keywords: type 2 diabetes mellitus, overweight, obesity, leptin, insulin
Chịu trách nhiệm chính: Nguyen Van Hoan
Ngày nhận bài: 8.11.2016
Ngày phản biện khoa học: 21.11.2016
Ngày duyệt bài: 1.12.2016
I. Introduction
Type 2 diabetes mellitus (T2DM) is achronic metabolic disorder withan exponential increase in developing countries.Theinternational diabetes federation (IDF) reported 382 million diabetes cases in 2013 with a prediction of 592 million cases by 2035, and 80% of these casesare in developing countries [1]. In Vietnam, the number of patients with T2DMis growingwith an estimated 3.3 million diabetes cases reported for 2014. The prevalence of diabetes in the age group of 30-69 yearsis estimated to be 5.7% across Vietnam and 7% in urban areas[2].
T2DMconstitutes up to 95% ofall diabetes and is characterized by chronic hyperglycaemia resulting from defects in insulin secretion and/or insulin action and metabolic disorders of protein and lipids [3]. The pathogenesis of T2DM consists of two major abnormalities including insulin resistance and dysfunction of insulin production,which lead to the disability to regulate blood glucose level [4]. The damage of pancreatic β cells to produce sufficient insulin andadiponectin as well as an increased production of pro-inflammatory cytokines due to obesity are the major contributing factors for T2DM [3]. Insulin resistance appeared years before the clinical manifestation of T2DM and is significantly associated with obesity, especially with abdominal and visceral obesity with an abnormally increased waist-to-hip ratio (WHR), dyslipidemia, hypertension and other metabolic disorders.Therefore, obesity largely contributes to insulin resistance in patients with T2DM[5].
Adipose tissueis recently recognized as an organ for metabolism of sexual steroids and production of adipsin that significantly contributes to loss of body weight [6]. Adipose tissue-derived proteins regulatemetabolic functionalities including hormone activities [7].Adipose tissueis also known as an endocrine organ that can produce various peptides with bioactivities namely adipokines. Increased adipose tissue due to obesity, especially deposition of visceral fat, is associated with insulin resistance, increased blood glucose levels, lipid metabolic disorders, hypertension and inflammation [7]. The adipose tissue-derived hormones such as adiponectin, leptin, adipsin, and resistin have been shown to be associated with metabolic disorders and are risk factors for T2DM and cardiovascular diseases. This study aims to investigate the levels of leptin andtheir correlations with insulin resistance ofoverweight/obese andT2DM.
II. MATERIALS AND METHODS
1.Patients and controls
One hundred thirty (n=130) patients with T2DMand one hundred twenty five (n=125) control individuals were included in the study. The patients were classified into two subgroups based on their BMI and T2DM status. The first subgroupincludes the patients with both overweight/obese (BMI³23) and T2DM (patients with overweight T2DM, n=57). The second subgroup includes patients with T2DM butwithout overweight (BMI<23)(non-overweight T2DM, n=73).The patients were diagnosed for T2DMbased on the standard criteria reported byworld health organization (WHO)in 1998 and byInternational Diabetes Federation (IDF) in 2005.The anthropometric indicators such as height, weight, waist and hip circumferencewere measured for all study participants.Body mass index (BMI) and waist-hip ratio (WHR) were calculated based on their anthropometric indicators(Table 1).
All the individuals in the control group were clinically examined and were considered healthy during sampling. None of them had any chronic infectious diseases or conditions such as hepatitis, liver cirrhosis, obstructive pulmonary disease, gout and/orany infection. The control group was also further divided intotwosubgroups. The first control subgroupincludenormal healthy individuals, (non-overweightcontrol individuals, n=57), with fasting venous blood glucose test <5.6 mmol/L, blood pressure <130mmHg and<85 mmHg, ECG in normal limits, other tests in the normal range, BMI from 18.5 to 23. The second control subgroup is healthy individuals with BMI³23(overweight/obese control individuals, n=68), fasting venous blood glucose test <5.6 mmol/L, blood pressure <130mmHg, and <85 mmHg, ECG in normal limits (Table 1).
2. Measurement of biochemical parameters
The levels of lipid components including cholesterol (CT), triglycerides (TG), high-density lipoprotein – cholesterol (HDL-C), low-density lipoprotein – cholesterol (LDL-C) were measured by using automatic biochemical AVADIA 1800(Siemens, USA). Fasting glucose levels were measured in bloodby measurement of the UV with Hexokinase.Insulin levels were measured by the Achitech i2000SR(Abbott, USA). Blood fasting glycosylated hemoglobin(HbA1c) levels were quantified by theion-exchange method using high performance liquid chromatography (HPLC).Insulin resistance index was evaluated according to the homeostasis model assessment insulinresistanceindex (HOMA-IR index) and the quantitative insulin sensitivity check insulinresistanceindex(QUICK-IR index).In addition, the β-cell function(homeostatic model assessment-HOMA-β) and the insulin secretion of β-cell were evaluatedaccording to Matthews’ method.
3. Measurement of leptin levels
The levels ofleptin were measured in the respective plasma samples ofthe study participants by using a commercial ELISAkit following the manufacturer’s instruction (Human leptin,Sigma,USA).
4. Statisticalanalysis
Clinical and demographic data were presented in median values with range for continuous variables.The student’s t-tests or one-way ANOVA were used for comparing mean of two or more groups, respectively. Chi-square or Fisher’s exact tests were used to compare categorical variables. Kruskal-Wallis or Mann-Whitney U test was used to analyze the plasma levels of leptininthe patients withT2DM and in controls wherever appropriate. All statistical analyses were performed using IBM Statistics SPSS v.19 (IBM Corp, Armonk, NY. the USA),and the level of significance was set at a P value of less than 0.05.
III. RÉULT
1.Demographic, clinical and biochemical characteristics of the study subjects
Table 1: Characteristics of patients with type 2 diabetes mellitus and controls
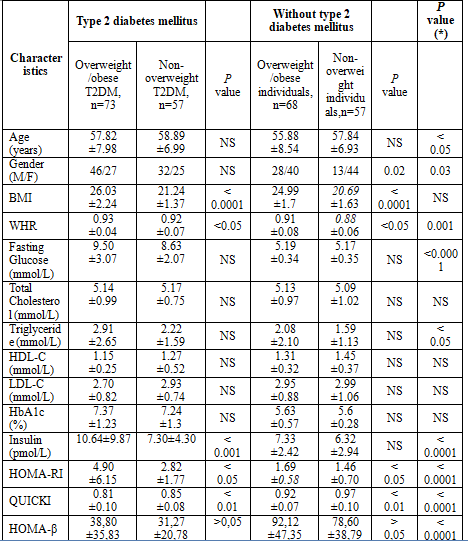 (*) Comparison between type 2 diabetes mellitus and non-diabetes mellitus.
(*) Comparison between type 2 diabetes mellitus and non-diabetes mellitus.
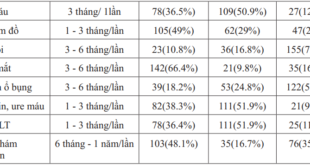
The demographic, clinical and biochemical characteristics of the patients with T2DM and controls are summarized in table 1. The mean age of the patients with T2DM was higher than control individuals (without T2DM) (P<0.05), while there was no difference of mean age between the patients with overweight T2DM and non-overweight T2DM. The proportion of males in the patients with T2DM was higher than the control group (P=0.03).
The levels of fasting glucose, triglycerideswere significantly higher in the patients with T2DM compared to control individuals (P<0.05). The levels of insulin and homeostasis model assessment insulin resistance (HOMA-RI) were significantly higher in the patients with T2DM compared to control individuals (P<0.001). Incontrast, the levels of quantitative insulin sensitivity check index (QUICKI) and homeostatic model assessment- β-cell function (HOMA-β) were significantly lower in the patients with T2DM compared to control individuals (P<0.001). (table 1).
2. Leptin levels in patients with type 2 diabetes mellitus and in controls
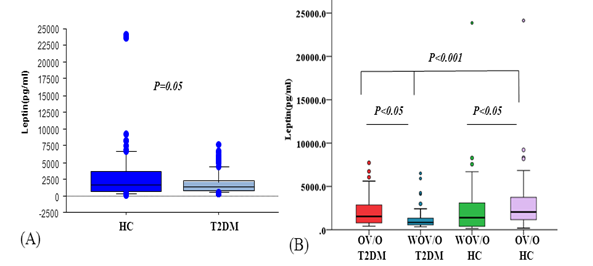
Figure 1: Leptin level in type 2 diabetes mellitus (T2D) patients
and heathy controls (HC).
(A) Leptin level was measured in the plasma of patients with T2DM and healthy controls and was compared between groups. (B) Leptin level in patients with overweight/obese (OV/O) T2DM and those with without overweight/obese (WOV/O) T2DM and in OV/O and WOV/O control individuals. P values were calculated by using Mann-Whitney U test.
The leptin levels were significantly lower in the patients with T2DM [median: 1202.75 pg/ml] compared to the controls [median: 1715.4 pg/ml] (P=0.05) (Figure 1A). Among the patients with T2DM, the leptin levels were significantly lower in the T2DM patients with WOV/O compared to those with OV/O T2DM (P<0.05). Among the control group, the leptin levels were significantly increased in the overweight/obese individuals compared to the WOV/O individuals (P<0.05)(Figure1B).
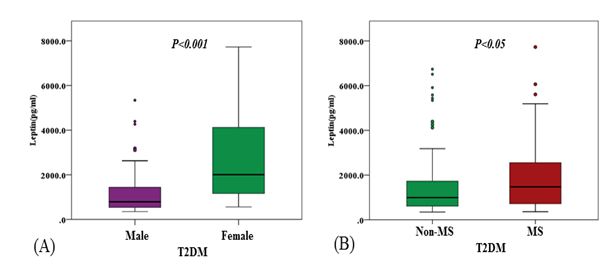
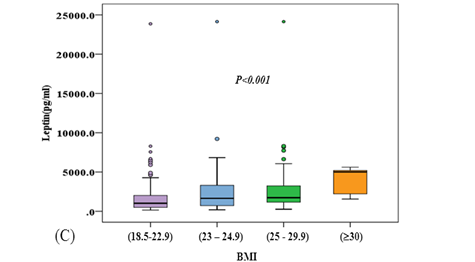
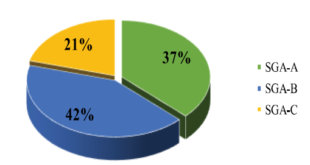
Figure 2: Leptin level in male and female patients with T2DM, in the T2DM patients with and without matabolic syndrome (MS) and in overweight/obese levels of subjects.
The levels of leptin were significantly increased in female patients with T2DM and in T2DM patients with metabolic syndrome(MS) compared to those of male patients (P<0.001) and T2DM patients with none-MS (P<0.05) (Figure 2A and 2B). The levels of leptin were significantly increased associated to BMI of subjects(p<0.001) (Figure 2C).
Discussion
Leptin, a hormone secreted by adipocytes in quantities which mainly reflect fat mass and serves as an important signal of body energy stores. Leptin deficiency in mice and/or in humans is associated with neuroendocrine and metabolic abnormalities, including insulin resistance and diabetes. All these abnormalities are corrected by exogenous leptin administration, suggesting that leptin plays a role in glucose homeostasis and possibly in the pathogenesis of other obesity-related metabolic complications [4].
Previous studies have shown that plasma leptin levels are closely associated with adiposity [8], and its level correlated with increased MS components [9]. Plasma leptin level in diabetes is rather controversial; one recent study does not observe any significant difference between diabetic and non-diabetic subjects, others reported significant lower level in type 1 diabetic subjects and type 2 diabetics with similar adiposity [10].In line with other studies, our results revealed that leptin levels were significantly increased in OV/Opatients with T2DM and in OV/O healthy individuals compared to patients with WOV/O T2DM and healthy individuals, respectively (Figure 1). In addition, our investigations revealed that leptin levels were increased female T2DM patients and in T2MS patients with MS. The increasing leptin levels were association to BMI of subjects (Figure 2). These results indicate that increased leptin may potentially respondedto the development of overweight/obese and T2DM and metabolic disorders.
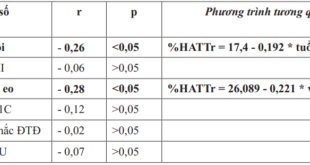
Recently studies shown that low leptin levels were also associated with the pathogenesis of many other diseases such as lipid metabolic disorders and obesity. Theleptin level was significant correlated to T2DM clinical parameters including insulin (r=0.23, p<0.05) and HOMA-β (r=0.216, p<0.05) and inversity correlated to QUICKI (r=- 0.366, p<0.0001).However, our data show that theleptin levels are not correlated with numerous clinical parameters such as triglycerides, cholesterol, HDL-C and LDL-C (data not shown). Those observations indicate that adiponectin levels involve in the development of T2DM.Therefore, based on the levels of leptin an adipose-derive cytokine could be useful for diagnosis of insulin resistance. However, more studies are required to propose a new index and verify the diagnostic accuracy in clinical practice and to establish a cut-off value and reference range of insulin sensitivity for specific populations [11].
Conclusion
Our study demonstrated that the levels of leptin are significantly modulated during the development of overweight/obese and T2DM. The leptin levels were significantly associated to BMI, genders and MS and with clinical parameters of obesity and T2DM. Leptin may possibly modulate the pathogenesis of overweight and T2DM.
Acknowledgements
We thank all the study subjects for their participation. This research is funded by Vietnam National Foundation for Science and Technology Development (NAFOSTED) under grant number106-YS.02-2014.36.
References
- IDF. Annual Report. 6th Edition. 2013.
- Pham,N.M. & Eggleston,K. Diabetes prevalence and risk factors among vietnamese adults: findings from community-based screening programs. Diabetes Care 2015; 38: e77-e78.
- Donath,M.Y. & Shoelson, S.E. Type 2 diabetes as an inflammatory disease. Rev. Immunol. 2011; 11: 98-107.
- Kahn,S.E., Hull,R.L., & Utzschneider,K.M. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature 2006; 444: 840-846.
- Guilherme,A., Virbasius,J.V., Puri,V. et al. Adipocyte dysfunctions linking obesity to insulin resistance and type 2 diabetes. Rev. Mol Cell Biol 2008; 9: 367-377.
- Kershaw,E.E. & Flier,J.S. Adipose tissue as an endocrine organ. J Clin. Endocrinol. Metab 2004; 89: 2548-2556.
- Jung,U.J. & Choi,M.S. Obesity and its metabolic complications: the role of adipokines and the relationship between obesity, inflammation, insulin resistance, dyslipidemia and nonalcoholic fatty liver disease. J Mol Sci 2014; 15: 6184-6223.
- Matsuzawa,Y., Hibi,K., & Kimura,K. Risk assessment for cardiovascular disease – microvascular dysfunction -. J 2010; 74: 1296-1297.
- Nishimura R, Sano H, Matsudaira T, Morimoto A, Miyashita Y, Shirasawa T, et al. Changes in body mass index, leptin and adiponectin in Japanese children during a three-year follow-up period: a population-based cohort study. Cardiovasc Diabetol. 2009;8:30.
Abu-Farha M, Behbehani K, Elkum N. Comprehensive analysis of circulating adipokines and hsCRP association with cardiovascular disease risk factors and metabolic syndrome in Arabs. Cardiovasc Diabetol. 2014;13:76.- Tatti P, Masselli L, Buonanno A, Di Mauro P, Strollo F. Leptin levels in diabetic and nondiabetic subjects. Endocrine. 2001;15(3):305–8.
 Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam
Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam