ABNORMAL THYROID FUNCTION IN NONTHYROIDAL ILLNESS
Tran Thi Bich Thuy, MD
Trieu An Hospital, Ho Chi Minh City
SUMMARY
Euthyroid sick syndrome can be described as abnormal findings on thyroid function tests that occur in the setting of a nonthyroidal illness (NTI), without preexisting hypothalamic-pituitary and thyroid gland dysfunction. Multiple alterations in serum thyroid function test findings have been recognized in patients with a wide variety of NTIs without evidence of preexisting thyroid or hypothalamic-pituitary disease. The most prominent alterations are low serum triiodothyronine (T3) and elevated reverse T3 (rT3), leading to the general term “low T3 syndrome.” Thyroid-stimulating hormone (TSH), thyroxine (T4), free T4 (FT4), and free T4 index (FTI) also are affected in variable degrees based on the severity and duration of the NTI. As the severity of the NTI increases, both serum T3 and T4 levels drop and gradually normalize as the patient recovers. Despite these abnormalities, treatment of these patients with thyroid hormone, while controversial, appears to be of little benefit and may be harmful. It is possible that the changes in thyroid function during severe illness are protective in that they prevent excessive tissue catabolism.
Key words: T4 (thyroxine), T3 (triiodothyronine), TSH (thyroid stimulating hormone), TRH (thyrotropin releasing hormone), D1(deiodinase 1), D2(deiodinase 2), D3 (deiodinase 3).
Main correspondence: Tran Thi Bich
Submission date: 1st August 2018
Revised date: 18th August 2018
Acceptance date: 31th August 2018
INTRODUCTION
The abnormal thyroid function is described among patients hospitalized in an intensive care unit. Although with the laboratory abnormalities, they had no thyroid gland diseases. There are terms used to describe that: Euthyroid sick syndrome (ESS), Non thyroidal illness syndrome (NTIS), Thyroid allostasis in critical illness-tumours-Uremia and starvation (TACITUS), Low T3 T4 syndrome, Low T3 syndrome.
Mild thyroid disease is very common and may present with only vague non-specific symptoms, especially in the elderly. Such patients can be performed thyroid function tests, the results of these tests become proplematic when being performed in patiens who have any significant co-existing illness (organic or psychiatric).
Changes of thyroid function tests may be: low T3,low FT3, high rT3, normal or low T4 normal or low FT4, normal or low or high TSH.
REVIEW OF HYPOTHALAMUS – PITUITARY -THYROID AXIS AND THYROID HORMONE METABOLISM
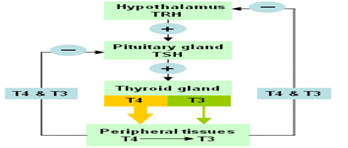
Figure 1. Regulation of Hypothalamus – Pituitary -Thyroid axis
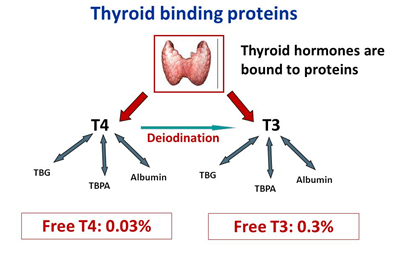
Figure 2. Thyroid binding proteins
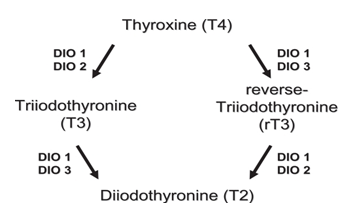
Figure 3. Thyroid hormone metabolism in health
TYPES OF CHANGES OF THYROID FUNCTION TESTS IN NON THYROIDAL ILLNESS
- Low T3 syndrome
- Low T4 syndrome
- TSH changes
Low T3 syndrome
The majority of hospitalized patients have low serum T3 concentrations, as some patients who are ill. There are often low total T3, low FT3, high rT3. Changing in T4 and TSH if the patients are more severe.
Low T4 syndrome
From 15 to 20% of hospitalized patients and up to 50% patients in Intensive care units have low serum T4 syndrome: reduced total T4, normal free T4 in patients not too severe.
TSH changes
Almost all patients have low TSH but detectable, greater than 0.05mU/L but less than 0.3 mU/L.
MECHANISM OF CHANGES OF THYROID FUNCTION TESTS IN NON THYROIDAL ILLNESS
Several mechanisms of low T3:
- High endogenous serum cortisol and exogenous glucocorticoids therapy.
- Circulating inhibitors of deiodinase activity, such as free (non- esterified) fatty acids.
- Treatment with drugs that inhibit 5’ monodeiodinase activity, such as amiodarone and high doses of propranolol.
- Cytokines (such as Tumor necrosis factor, Interferon –alpha, NF-kB, Interleukin 6)
- Impaired uptake T4 into hepatocyte reducing the availability of substrate for conversion to T3.
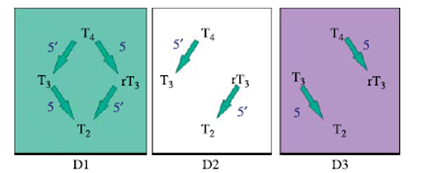
Figure 4. Deiodination reactions catalyzed by the iodothyronine deiodinase
isoenzymes D1, D2, D3
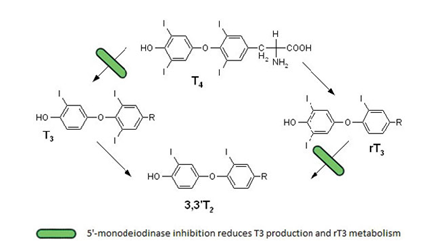
Figure 5. Deiodination reactions in Non thyroidal illness syndrome
Mechanism of low T4:
- Reduction of one or more of thyroid hormone proteins:
- TBG (thyroxine binding protein): major binding protein, decreased production of normal TBG or production of TBG that binds T4 poorly because it is abnormally glycosylated or is cleaved in the circulation.
- TTR (transthyretin) or TBPA (thyroxin binding prealbumin)
- Albumin
- Inhibitors of T4 binding such as free fatty acid, salicylate, furosemide…
Changes of TSH
Medications used for hospitalized patients can cause suppression of TSH secretion such as Doputamine, Glucocorticoids, octreotide.
MAPK (Mitogen Activate ProteinKinase), JAK (Janus Kinase), STAT (Signal Transducer & Activator of Transcription), GSH (Glutamin cysteinylglycine)
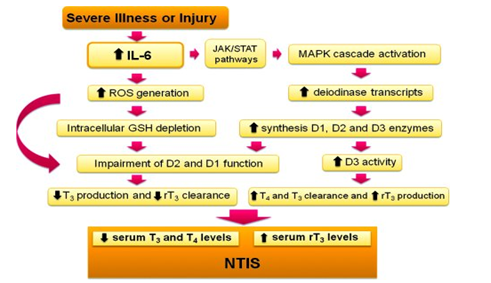
Figure 6. Mechanisms of thyroid hormones in Non thyroidal illness
Transient central hypothyroidism
Patients with severe non thyroidal illness may have acquired transient central hypothyroidism. This suggestion is support by the following observations:
- A prospective study evaluated changes in thyroid function in patients undergoing bone marrow transplantation: TSH fell coincident with declines in T4
- A study of critically ill patients recovering from non thyroidal illness demonstrated that a rise TSH (which transiently reached supranormal values in some patients) preceded normalization of
- Patients with non thyroidal illness, similar to those with central hypothyroidism from other causes, have a blunted nocturnal rise TSH, but usually have a normal TSH response to TRH (thyrotropin releasing hormone).
- Abnormalities in TSH glycosylation that may decrease TSH bioactivity have been found in patients with non thyroidal illness and also in patients with central hypothyroidism.
- TRH mRNA in the paraventricular nucleus of the hypothalamus was reduced in patients who died with non thyroidal illness and was correlated with premortum T3 and TSH.
- TRH (protirelin) infusion in patients with critical illness raises TSH, T4 and T4.
- Infusion of interferon – alfa to 8 normal men caused a fall in TSH, T3 as well as a rise rT3 and interleukin 6, thus mimicking the thyroid metabolic changes of serious illness, except that there were no fall in T4.
- Animal studies support the hypo thesis that inflammation (eg injection of endotoxin in rodents) upregulates hypothalamic deodinase D2, which increases local T3 production and lowers TRHmRNA expression.
MSH (Melanocyte stimulating Hormone), NPY (Neuropeptide Y),
AGRP (Agouti related Protein), ARC (Arcuate nucleus), PVN (ParaVentricular Nucleus), GABA (gamma amino butyric acid)
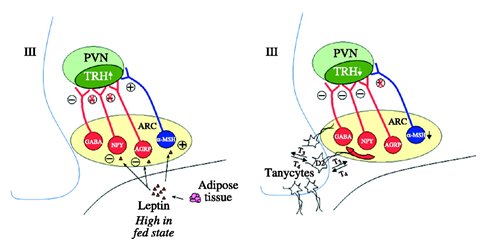
Figure 7. Proposed mechanism behind the central hypothyroidism (low TRH) induced by the non thyroidal illness and fasting
The neurons of PVN that secrete TRH are innervated by neurons from the ARC that contain MSH, NPY, AGRP and GABA. Both NPY and AGRP inhibit TRH gene expression, an action prevented by leptin.
- During fasting, when leptin decreases, the inhibitory action of NPY and AGRP can prevail leading to diminished TRH. The expression of TRH in the PVN is stimulated by MSH, and this effect is enhanced by leptin. Thus, in fasting (low leptin), the stimulatory action of MSH on TRH expression in the PVN is diminished.
- Sepsis or inflammation: T3 produced by iodothyronine deiodinase D2 in tanycytes has important feedback inhibitory actions on TRH production in PVN. During sepsis and trauma, there is an increase in tanycyte D2, which is postulated to lead to an increased generation of T3 from T4.
Different mechanisms
- The expression of the selenoenzymes D1, D2, D3 may be limited by the low selenium supply in patients with severe illness or sepsis.
- Impaired thyroid hormone uptake by tissue may be caused by depletion of ATP or the presence in plasma of substances that impair hepatic uptake of thyroid hormone.
- Some other complicated mechanisms are related to thyroid hormone receptors and the role of thyroid hormone transporters.
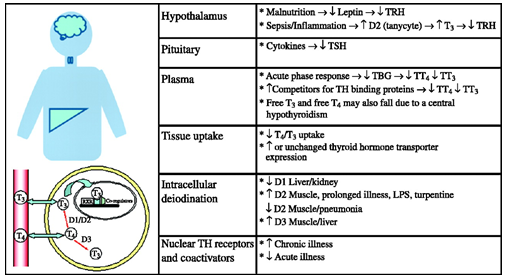
Figure 8. Summary of the mechanism that lead to thyroid hormone changes in non thyroidal illness syndrome.
PROGRESSION AND PROGNOSIS
The magnitude of the changes in thyroid function in patients with non thyroidal illness varies with the severity of the illness. T4 value correlates with outcome. When a patient recovers from illness, abnormalities in serum TSH and thyroid hormone concentrations eventually resolve. In some patients, however, TSH may rise transiently above the reference range in this recovery phase.
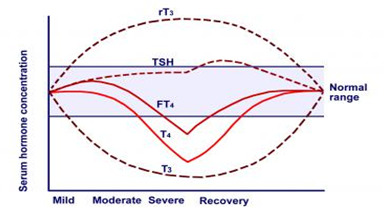
Figure 9. Schema showing the general changes that occur in serum thyroid –related hormones following illness of varying severity.
TREATMENT
- In critically ill patients with low T3 and/or T4 and no other clinical signs of hypothyroidism, we suggest not treating with thyroid hormone (grade 2B).
- In previously euthyroid patients undergoing coronary artery bypass graft (CABG), we recommend not treating with thyroid hormone in the immediate post operative period (grade 1A).
- If there is additional evidence to suggest a diagnosis of hypothyroidism in critically ill patients, we suggest that patients receive the thyroid hormone (grade 2C). In the absence of suspected myxedema coma, repletion should be cautious, beginning with approximately half the expected full replacement dose of T4.
CONCLUSIONS
Assessment of thyroid function in patients with non thyroidal illness is difficult, especially among those hospitalized in an intensive care unit. Many of them have low T4, free T4, T3, and their serum TSH may also be low. The mechanisms behind the hormone changes seen in non thyroidal illness are now becoming clearer, the changes represent a physiological adaptation, attempts to restore thyroid hormone levels could even have adverse effects on patient outcome.
REFERENCES
- Douglas S Ross , David S Cooper, Jean E Mulder. Thyroid function in nonthyroidal illness. uptodate.com 2017
- Maria H Warner & Geoffrey J Beckett. Mechanisms behind the non –thyroidal illness syndrome. Journal of endo. (2010) 205, 1-13
- Wikipedia 2009. Euthyroid sick syndrome
- Simone Magagnin Wajner& Anna Luiza Maia. New insights toward the acute non thyroid illness syndrome. Front. Endocrinol., 26 January 2012 https://doi.org/10.3389/fendo.2012.0008.
- Serhat Aytug, Romesh Khardori. Euthyroid sick syndrome. Updated Apr 27, 2017.
- 6.Luca F, Goichot B, Brue T. Non thyroidal illnesses (NTIS). Ann Endocrinol (Paris) 2010;71 (Suppl 1) S 13- 24.
- Economidou F, Douka E, Tzanela M, Nanas S, Kotanidou A. Thyroid function during critical illness. Hormones 2011;10 (2) 117-124.
- Bello G, Ceaichisciuc I, Silva S, Antonelli M. The role of thyroid dysfunction in the critically ill: a review of literature. Minerva Anestesiol 2010;76 (11) 919-928.
- Magagnin Wajner S, Maia AL. New insights toward the acute non thyroidal illness syndrome. Front Endocrinol 2012;3 (8) 1-7 Epub 26 Jan 2012
- Wang F, Pan W, Wang H, Wang S, Pan S,Ge J. Relationship between thyroid function and ICU mortality: a prospective observation study. Crit Care 2012;16 (1) R11.
- Bello G, Pennisi MA, Montini L, Silva S, Maviglia R, Cavallaro F, Bianchi A, De Marinis L, Antonelli M. Nonthyroidal illness syndrome and prolonged mechanical ventilation in patients admitted to the ICU. Chest 2009;135 (6) 1448-1454.
- Mancini A, Festa R, Di Donna V, Leone E, Littarru GP, Silvestrini A, Meucci E, Pontecorvi A. Hormones and antioxidant systems: role of pituitary and pituitary-dependent axes. J Endocrinol Invest 2010;33 (6) 422-433.
 Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam
Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam