ASSESSEMENT OF FALL RISKS AND RELATIVES IN ELDERLY TYPE 2 DIABETIC PATIENTS AT NATIONAL GERIATIC HOSPITAL
*Lê Anh Tú,**Nguyễn Xuân Thanh, **,***Nguyễn Ngọc Tâm, **,***Vũ Thị Thanh Huyền
*Nghe An Endocrinology Hospital,*National Geriatric Hospital,*Ha Noi Medical University
Corresponding author: Vu Thi Thanh Huyen
SUMMARY
Aims: Assessment of fall risk and related factors in elderly type 2 diabetic patients. Subjects and methods: A cross sectional study included of 412 elderly type 2 diabetic patients diagnosedwith diabetes according to WHO 2006 criteria. The patients were interviewed, are assessed for fall risk and other related factors. Results: Average age: 71.9 ± 7.6 years, female/male ratio: 1.3. Of total 421 elderly type 2 diabetic patients, the proportion of high risk and low risk of fall was 26% and 74%, respectively. There were positive relationships between advanced age and duration of diabetes with risk of fall in elderly type 2 diabetic patients (r > 0.5; p < 0.05). There were no correlations between blood glucose,or HbA1c with risk of fall in elderly type 2 diabetic patients (r < 0.25; p > 0.05). Conclusion: Elderly type 2 diabetic patients had high risk of fall, especially in those with advanced age and longer duration of diabetes
Key words:Type 2 diabetic patients, elderly, fall risk.
Main correspondence:Le Anh Tu
Submission date:9 Feb 2017
Revised date:21 Feb 2017
Acceptance date: 15Mar 2017
I. INTRODUCTION
The elderly population worldwide is increasing, accounting for about 8.3% of the world population and is expected up to 30% in 2050 [1]. Vietnam is a country with an aging population trend, the percentage of elderly people as reported in 2009 was 9.5%, and will be projected to 16.8% in 2029[2]. Of chronic diseases, the diabetes have a high prevalence in the elderly (> 10%). The risk of mortalily is doubled in diabetic elderly compared to those in non-diabetic elderly. Diabetes is the most important risk factors of functional impairment in older people [3]. In addition to micro- and macrovascular complications, elderly diabetic people are also at risk for other complications such as depression, cognitive impairment, muscle atrophy, falls, fractures…
Some study also showed that diabetes is one of the important predictors of the risk of falls. The result of the Study of Osteoporotic The study Fractures including of 9247 women aged 67 and older, showed that 18% of older women fell more than once a year. Research has shown that diabetic patients including insulin naive or insulin treatment may increase the risk of falls than those without diabetes [4].
Falls can lead to fractures, reduced glycemic control and reduced quality of life in patients with diabetes. Additionally, fall could cause post-fall syndrome characterized by anxiety, decrease physical and social activites. The number of researches on fall risks and related factors on elderly diabetic patients have been limited in Viet Nam. Hence, we conduct the study to assess of risk fall and related factors in elderly type 2 diabetic patients.
II. SUBJECTS AND METHODS
2.1. Subjects
Inclusion criteria: Type 2 diabetic patients above 60 years old diagnosed diabetes according to WHO 2006 criteria were examined and treated in National Geriatric Hospital. Exclusion criteria: Patients with severe complications such as: stroke, acute heart failure, diabetic ketoacidosis, hyperosmolar hyperglycemic nonketoacid syndrome, … Patients or their family members did not agree to join in study.
2.2. Study design:
Descriptive cross-sectional study.
2.3. Study variables:
Socio-demographic variableswere measured such as current age (60-69 years, 70-79 years, >80 years), gender (male, female), education level (lower high school, complete high school, superieur), marital status (live with wife/husband, live alone).
The Hendrich II Fall Risk Model (HIIFRM)was used to to assess the risk of falls in the study subjects[5]. Process of implementation was following: interviewing the patients about the risks and medications may cause fall, conducting “Get up and go” test[6]: the patients sit on a chair, investigator asked the patients to stand up and go 3 meters and turn back to the seat. The total time (by seconds) for patients completing the task was recorded. The results corresponded to patients’ answering questions and performing tests according to risk assessment tables was recorded. If total points less than 5 points, subject had no risk of falls, if total points was 5 points and more, subject had high risk of fall.
Assessment of related factors: gender, age, fasting blood glucose levels, HbA1C and duration of diabetes (5 years, 5-10 years, > 10 years). Grouping of good and not good blood glucose control based on fasting blood glucose ≤ 7,2 mmol/l, HbA1c <7%, and fasting blood glucose levels > 7.2 mmol/L and HbA1C ≥ 7%, respectively.
2.4. Statistical analysis
Analysis of the data was performed using SPSS for Windows 16.0. Continuous variables was presented as mean ± standard deviation, and categorical variables as frequency and percentage. Statistical analysis was performed through the test: Chi-square tests for categorical variables and Student’s t-tests or Mann-Whitney tests for continuous variables. Two-tailed P values < 0.05 were considered statistically significant.
III. RESULTS
3.1. Characteristics of the study participants
A total of 412 participants were recruited from Octorber 2015 to Octorber 2016. They had a mean age of 71.9 ± 7.6 (60 – 91 years), proportion of participants aged 70 years and older was 57.3%.
Table 1. Characteristics of the study participants (n=412)
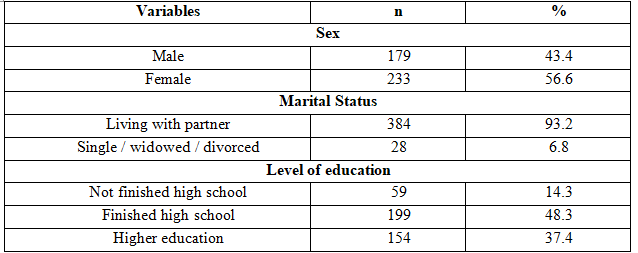 In the study, prevalence of male was 43.4%, lower than prevalence of female (56.6%). The prevalence of participants finishing high school or had higher education was quite high (86.7%). Almost patients was living with partner (93.2%).
In the study, prevalence of male was 43.4%, lower than prevalence of female (56.6%). The prevalence of participants finishing high school or had higher education was quite high (86.7%). Almost patients was living with partner (93.2%).
3.2. Assessing the high risk of falls and some related factors in the study participants
Table 2: Fall risk assessment in the study participants
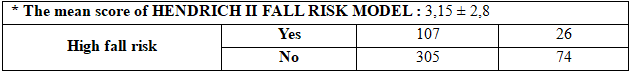 The average score of the Hendrich II fall risk model was 3,15 ± 2,8. The proportion of patients had high fall risk was 26% according to The Hendrich II fall risk model.
The average score of the Hendrich II fall risk model was 3,15 ± 2,8. The proportion of patients had high fall risk was 26% according to The Hendrich II fall risk model.
Table 3. Factors associated with high fall risk
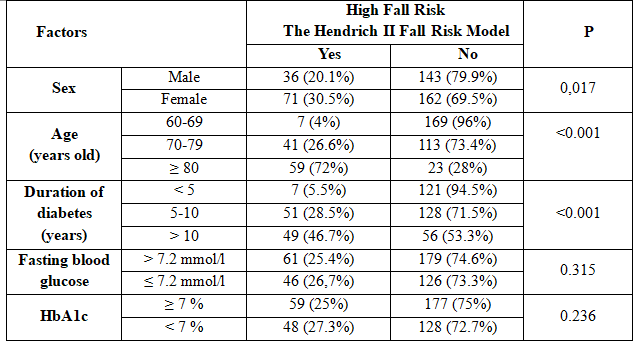 The results showed that female had higher fall risk (30.5%) than male (20.1%). There was a correlation between patient’s fall risk and sex with p < 0.05. There was a higher proportion of high fall risk in over 80 year-old group than 70-79 year-old and 60-69 year-old group (72% versus 26.6% and 4%, respectively) with p <0.05. The percentage of high risk of falls in the group with 10-year duration of diabetes was 46.7%; higher than that in the group with 5-10 year duration of diabetes (28.5%) and less than 5-year duration of diabetes (5.5%) (p <0.05).
The results showed that female had higher fall risk (30.5%) than male (20.1%). There was a correlation between patient’s fall risk and sex with p < 0.05. There was a higher proportion of high fall risk in over 80 year-old group than 70-79 year-old and 60-69 year-old group (72% versus 26.6% and 4%, respectively) with p <0.05. The percentage of high risk of falls in the group with 10-year duration of diabetes was 46.7%; higher than that in the group with 5-10 year duration of diabetes (28.5%) and less than 5-year duration of diabetes (5.5%) (p <0.05).
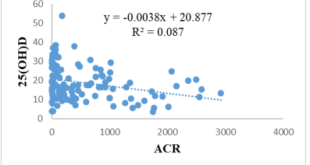
Table 4. The correlation between age, duration of diabetes, blood glucose levels, HbA1c and high fall risk
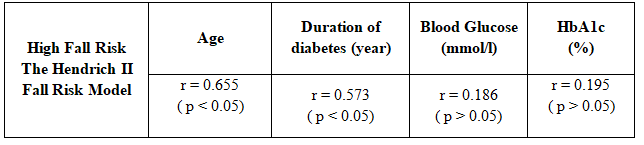 There was positive correlation between fall risk with duration of diabetes and advanced age (p < 0.05). There was no correlation between blood glucose, HbA1C and high fall risk in study participants (r <0.25; p > 0.05).
There was positive correlation between fall risk with duration of diabetes and advanced age (p < 0.05). There was no correlation between blood glucose, HbA1C and high fall risk in study participants (r <0.25; p > 0.05).
IV. DISCUSSION:
The patients in the study had a mean age of 71.9 ± 7.6 years old. Age group 60-69 accounted for the highest rate of 42.7%, the group aged 80 and older accounted for the lowest percentage of 19.9%. The average age in the study was similar to the study by Nguyen Thi Thu Huong, in which all patients aged 60 years or older were selected at National Geriatric Hospital, the average age of the patients was 70.2 ± 6.7 people, ages 60-69 accounted for the highest percentage of 49%[7].
Falls can lead to fractures, poor glycemic control and reduced quality of life in patients with diabetes. A study reported that diabetic patients tended to have poor balance during standing in the place with lack of light, and increased shaken during standing [8]. The results in this study showed that 26% patients had high fall risk. This proportion was the same with the study of Patil SS [9]conducted in India on 416 elderly people (29.8% had fall risk). The result was lower than the research on 50 diabetic patients in Brazil of Oliveira PP (72% had fall risk) [10].
There was a correlation between advanced age, duration of diabetes and high fall risk in elderly patients with type 2 diabetes. The advanced age group had the higher fall risk (r = 0,655, p < 0,05). The group aged 80 years old and older had the highest fall risk (72%). This results was the same as those from Rebecca K. Yau [11]. The reason can be explained by advanced age often increasing the risk of frailty, inmobility, decrease physical activities, capacities odd keeping balance.
In the study, female had the higher fall risk than male (30.5% and 20.1%, p < 0.05; OR = 1.74; 95% CI: 1.1-2.75). This results was similar with Rebecca K. Yau [11]. The reason behind this might be female has longer longevity and bone mass decline faster than female, especially in 5 years after menopause. In consequence, the ability of standing and keeping their balance was worse than that in male [12].
Diabetic duration had correlation with fall risk in elderly type 2 diabetic patients(r = 0.573; p < 0.05). Proportion of high fall risk in group with diabetic duration more than 10 years was 46.7%, higher than group with 5-10 year duration of diabetes (55%), p < 0.05. The results was similar to Rebecca K. Yau’s study [133].
Provided that patients with long-time diabetes had an increased risk of falls. This may be due to patients with type 2 diabetes with risks for long-term and advanced complications, including peripheral neuropathies and diabetic foot diseases; The main factors causing the decline in peripheral sensory and reaction time led to declining ability to hold the body when walking on uneven surfaces, thereby increasing the risk of falls [13].
The results has not showed an association between risk of falls and blood glucose control in the study groups. This were similar to Miller DK’s research[14] showing no association between fall and poor glycemic control, while some studies had evaluated the association between glycemic control poor and down [134].
On the other hand, hypoglycemia as well as insulin treatment has been shown to be risk factors for increasing falls in elderly diabetic patients. For this reasons, further research, especially on disease intervention in elderly diabetic people are needed to more clearly define the relationship between glycemic control and risk of falls.
V. CONCLUSION
Elderly type 2 diabetic patients had higher risk of fall. The risk of fall was higher in patients who had higher age and diabetic duration.
REFERENCES
- Inter-Ministerial Committee on Aging Report (1999), Misnistry of Community Development, Singapore.
- UNFPA Viet Nam(2011), The aging population in Viet Nam: Current status, prognosis and possible policy responses.
- Meneilly GS (2006), “Diabetes in the Elderly“, Medical clinics of North America – Geriatric medicine, Vol.90, tr. 909-923.
- Schwartz AV, Hillier TA, Sellmeyer DE và các cộng sự. (2002), “Older women with diabetes have a higher risk of falls: a prospective study“, Diabetes Care, 25, tr. 1749-1754.
- Hendrich, Bender và Nyhuis (2003), “Validation of the Hendrich II Fall Risk Model: A large concurrent case/control study of hospitalized patients.“, Applied Nursing Research, 16(1), tr. 9-21.
- Podsiadlo D và Richardson S (1991), “The Timed Up & Go: A test of basic functional mobility for frail elderly persons“, J Am Geriatr Soc, 39:142-148.
- Nguyen Thi Thu Huong (2013), Research on lipid metabolism disorders in diabetic elderly patients, MD thesis, Hanoi Medical University.
- Petrofsky JS, Cuneo M, Lee S và các cộng sự. (2006), “Correlation between gait and balance in people with and without Type 2 diabetes in normal and subdued light“, Med Sci Monit, 12: CR273–CR281.
- Patil SS, Suryanarayana SP, Dinesh R và các cộng sự. (2015), “Risk factors for falls among elderly: A community‑based study“, Int J Health Allied Sci, 4:135-40.
- Oliveira PP, Fachin SM, Tozatti J và các cộng sự. (2012), “Comparative analysis of risk for falls in patients with and without type 2 diabetes mellitus“, Rev Assoc Med Bras, 58(2):234-9.
- Rebecca K. Yau, Elsa S. Strotmeyer, Helaine E. Resnick và các cộng sự. (2013), “Diabetes and Risk of Hospitalized Fall Injury Among Older Adults“, Diabetes Care, 36(12):
3985-3991. - World Health Organization (2007), A Global Report on Falls Prevention Epidemiology of Falls, Canada.
- Menz HB, Lord SR, St George R và các cộng sự. (2004), “Walking stability and sensorimotor function in older people with diabetic peripheral neuropathy“, Arch Phys Med Rehabil, 85: 245–252.
- Miller DK, Lui LY, Perry HM 3rd và các cộng sự. (1999), “Reported and measured physical functioning in older inner-city diabetic African Americans“, J Gerontol A Biol Sci Med Sci, 54: M230–M236.
 Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam
Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam