MEDICATION ADHERENCE AND ASSOCIATED WITH HEMOGLOBIN A1C
IN TYPE 2 DIABETES
Nguyen Van Bang(1), Le Van Chi(2)
(1: Postgraduate student of Hue University of Medicine and Pharmacy
(2: Lecture of Hue University of Medicine and Pharmacy
ABSTRACT
Background: Diabetes mellitus (DM) is now one of the most common non-communicable diseases affecting the global population, with increasing incidence in many emerging countries of the world. 1% reduction in HbA1c is associated with 21% reduction in death related to T2DM, 14% reduction in myocardial infarction and 37% reduction in micro-vascular complications. However, in real practice, poor metabolic control among T2DM is often reported in the literature. Medication non-adherence is of increasing concern for healthcare providers despite the known benefits of modern treatment regimens, with prevalence reported in one study to be in excess of 50 % of diabetic patients. Objective: 1) To evaluate the general level of medication adherence in patients with type 2 diabetes by using MMAS-8. 2) To identify the correlation between demographic characteristics with medication adherence. 3) To find the associations between medication adherence and glycemic control. Methods: A total of 192 T2DM patients include 82 out-patients and 110 in-patients who was selected at Diabetes Out patient clinical room and admitted to the Endocrinology – Respiratory – Neurology Department, Hue Central Hospital, were evaluated in a Cross-sectional study from January 2015 to April 2017. Morisky scale, also known as Morisky Medication Adherence Scale (MMAS) was used for the assessment of medication adherence. Results: The average HbA1c was 9.1 ± 2.6%. The proportion of patients having poor glycemic control was 76.0% following HbA1c ≥7.0% criteria and 75.0% following Fasting glucose criteria, and the mean MMAS-8 score was 6.1 ± 1.6 out of a score range of 0-8. There were 51.0% who reported optimal medication adherence (MMA-8 > 6). There are significant association between demographic variables (living area, occupation, educational level), biochemical marker (HbA1c, fasting glucose, dyslipidemia) with medication adherence following MMAS-8. Higher medication adherence, good control fasting glucose are as statistical predictors of good glycemic control. Conclusions: Higher medication adherence, good control fasting glucose as statistical predictors of good glycemic control.
Keywords: medication adherence, MMAS-8, glycemic control, HbA1c, Fasting glucose
Main correspondence: Nguyen Van Bang
Submission date: 1st August 2018
Revised date: 18th August 2018
Acceptance date: 31th August 2018
I. INTRODUCTION
Diabetes mellitus (DM) is now one of the most common non-communicable diseases affecting the global population,with increasing incidence in many emerging countries of theworld[13]. According to the IDF 2014, it was estimated that 387 million people worldwide had DM, corresponding to a global prevalence of 8.3%[10]. In this context, type 2 diabetes mellitus (T2DM) accounts for the majority of these cases. T2DM is a serious public health concern becauseof the heavy financial and social cost of the management process. T2DM requires a lifetime of personal care, as it is adisease with serious short and long-term consequences forthe afflicted.
In clinical practices, maintenance of glycated hemoglobin levels (HbA1c) remains the major therapeutic objective for prevention of T2DM-related complications. HbA1c is the gold standard for monitoring T2DM, whereby higher values are associated with higher trends of developing cardiovascular complications. On the other hand, 1% reduction in HbA1c is associated with 21% reduction in death related to T2DM, 14% reduction in myocardial infarction and 37% reduction in micro-vascular complications [4]. However, in real practice, poor metabolic control among T2DM is often reported in the literature.
Medication non-adherence is of increasing concern for healthcare providers despite the known benefits of modern treatment regimens, with prevalence reported in one study to be in excess of 50 % of diabetic patients[6]. Some study show that for every 25% increase in MA, a patient’s HbA1c is reduced by 0.34%[14].
Medication non-adherence is also a costly economic burden worldwide with an estimated annual disease-related medical cost of USD 100 billion. Besides limiting the effectiveness of treatment and increasing healthcare costs medication non-adherence also leads to a rise in morbidity and mortality rates[7].
Various methods which have been used to assess medication adherence can be divided into direct methods (such as monitoring of serum drug levels and direct observation of therapy), and indirect methods (such as patient self-report, pill counts, rate of prescription refills, patient diaries and electronic container monitors)[7].
The Morisky, Green and Levine Scale has been commonly used for the assessment of medication adherence. This instrument was originally developed with 4 items only but has since been modified to the current 8-item Morisky Medication Adherence Scale[11], [12].
Objective:
The present study aimed:
- To evaluate the general level of medication adherence in patients with type 2 diabetes by using MMAS-8.
- To identify the correlation between demographic characteristics with medication adherence.
- To find the associations between medication adherence and glycemic control.
II. METHODS
Ethical approval
This study received approval from the Institutional Review Board of Hue University of Medicine and Pharmacy. Written consent was also obtained from the patients prior to the commencement of the study.
Participants and setting
A total of 192 T2DM patients include 82 out-patients and 110 in-patients who was selected at Diabetes Out patient clinical room and admitted to the Endocrinology – Respiratory – Neurology Department, Hue Central Hospital, were evaluated in a Cross-sectional study from January 2015 to April 2017. Patients were diagnosis DM following ADA 2015 criteria [5]
The inclusion criteria was (1) Patients diagnosed with type 2 diabetes at least 3 months before inclusion in the study, (2) Patients able to recognize their diabetes medications from the total medications that they have to take daily, (3) Patients willing to participate, who have given agreement to participate in the study.
The exclusion criteria was (1) patients unableto answer the questionnaire independently, without assistance from caregivers, (2) who lack biochemical examinations (FPG, HbA1c, lipid profile).
Data collection form
Data were collected using a set of questionnaires including demographic (age, sex, Employment status, Education level) and clinical variables (Diabetes duration, Diabetes medication, medication side effect, self glucose monitoring, diabetes complications, BMI, blood pressure and biochemical examinations) and treatment adherence (MMAS-8).
Medication adherence
Morisky scale, also known as Morisky Medication Adherence Scale (MMAS) was used for the assessment of medication adherence. The MMAS was translated into the Vietnamese language. MMAS consists of 8 items with a dichotomous response (yes/no) for items 1–7 and a 5 point Likert response for the last item. The total score ranges from 0 to 8 with a higher total score indicating higher medication adherence. The MMAS showed a good predictive power and was significantly associated with drug pharmacy refill as it showed a 75% concordance.
Glycemic control
HbA1C is a biochemical marker whose levels correlate with patient blood glucose levels over a defined time period (3 months) and measurement of HbA1C levels is an accurate way to assess glycemic control over a defined time period. The current study used HbA1C as an indicator of glycemic control among patients. As recommended by ADA 2015, HbA1C values equal and above 7% are indicative of poorly controlled glycemic levels, and thus poor diabetes management.
Procedure
Data collection was done by face-to-face interviews from the patients. No formal patients were helped to answer the questions. Medical records were reviewed for recent hemoglobin A1C (HbA1C) levels (within 3 months of the inclusion) retrospectively, FPG, lipid profile, diabetes complications, blood pressure.
Statistical analysis
Descriptive statistics were used to describe demographic and disease characteristics of the patients and their medication adherence scale. Percentages and frequencies were used for the categorical variables, while mean and standard deviations were calculated for the normally distributed continuous variables. Non-parametric statistical tests were used accordingly. Mann–Whitnney test and Kruskal–Wallis test were used to test the differences in the MMAS scores between groups.
Spearman correlation coefficient was used to identify relationship between adherence scores, demographic, clinical variables and HbA1C results Multivariate binary logistic regression analysis and adjusted odds ratios were used to identify factors predicting good glycemic control and patient medication adherence. P values less than 0.05 often fails to identify important variables. All statistical analyses were performed using SPSS version 16.0. The significance level was set at P less than 0.05.
III. RESULTS
Participant Characteristics
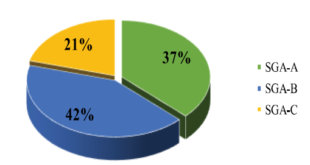
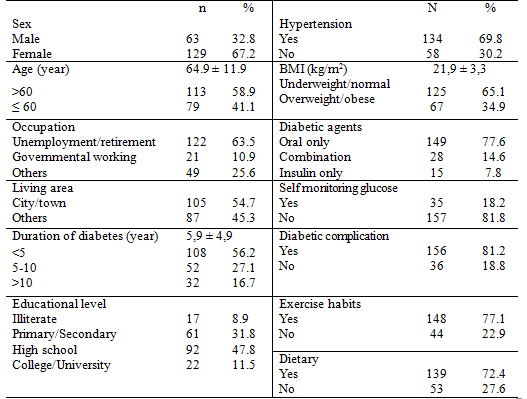
A total of 192 eligible patients completed the questionnaires. The average age was 64.9 ± 11.9 year, 58.9% than 60 year and 67.2% (129/192) were female subjects. More than half (54.7%) of these participants live in city/town and most of them (63.5%) were unemployment or retirement. 11,5% of patients attained their highest education at college/university/postgraduate.
The mean duration of diabetes was 5.9± 4.9 years. Proportion of patients who had hypertension, overweight/obese were 69.8% and 34.9%, respectively. Majority of patients were on combination oral anti-diabetes medicines (77.6%) and did not use insulin for their diabetes management. 81.2% of patients were recorded having diabete complications and most of them were using medical nutrition – exercise habits.
Table 1. Patient Characteristics (N = 192)
 Medication adherence and glycemic control
Medication adherence and glycemic control
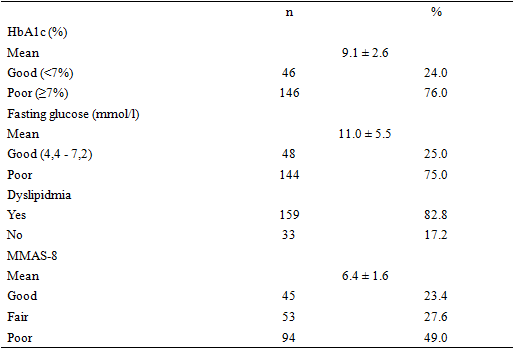
The average HbA1c was 9.1 ± 2.6%. The proportion of patients having poor glycemic control was 76.0% following HbA1c ≥7.0% criteria and 75.0% following Fasting glucose criteria, and the mean MMAS-8 score was 6.1 ± 1.6 out of a score range of 0-8. There were 51.0% who reported optimal medication adherence (MMA-8 >6) table 2.
Table 2. Medication adherence and glycemic control
 Patient Characteristics According to Medication adherence
Patient Characteristics According to Medication adherence
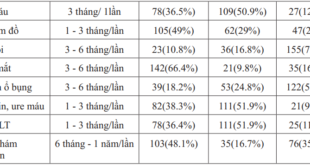
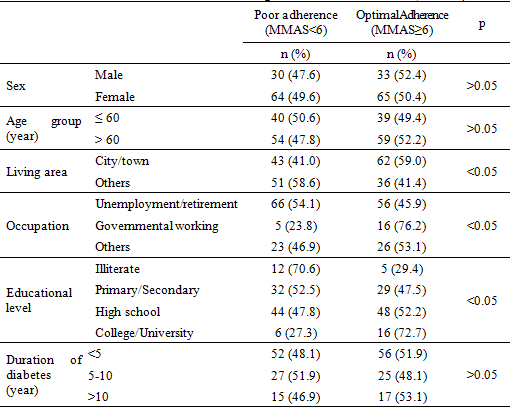
Table 3 and table 4 shows the distribution of demographic and clinical characteristics of the participants according to level of adherence (poor adherence and optimal adherence). A Chi-square test for independence indicated significant association between demographic variables (living area, occupation, educational level), biochemical marker (HbA1c, fasting glucose, dyslipidemia) with medication adherence following MMAS-8.
Table 3. Patient Characteristics According to Medication adherence (N = 192)
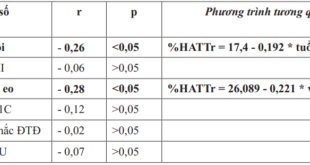
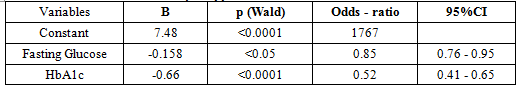
 When all predictors were included in the binary logistic model, only fasting glucose and HbA1c were found to be significantly associated with adherence. Clearly, a negative association between HbA1c levels, fasting glucose level and adherence were identified where a 1% reduce in HbA1c is associated with a 1.92 time increase in the likelihood of being adherent. A 1 mmol/l reduce in fasting glucose is associated with a 1.2 time increase in the likelihood of being adherent (table 5).
When all predictors were included in the binary logistic model, only fasting glucose and HbA1c were found to be significantly associated with adherence. Clearly, a negative association between HbA1c levels, fasting glucose level and adherence were identified where a 1% reduce in HbA1c is associated with a 1.92 time increase in the likelihood of being adherent. A 1 mmol/l reduce in fasting glucose is associated with a 1.2 time increase in the likelihood of being adherent (table 5).
Table 4. Patient clinical and biochemical marker According to Medication adherence
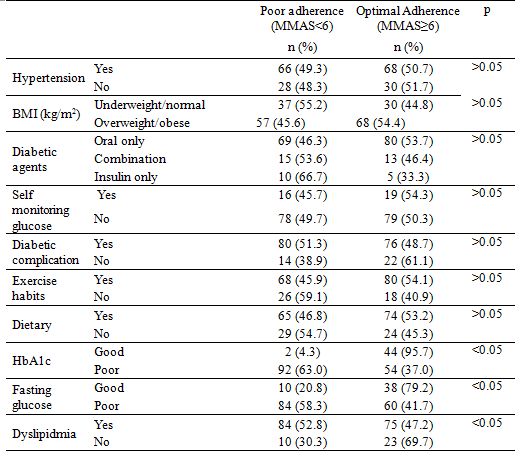 Table 5. Multivariate analysis of factors associated with medication adherence
Table 5. Multivariate analysis of factors associated with medication adherence
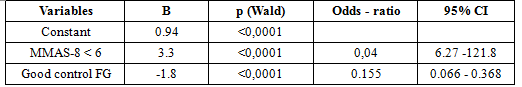
 Multiple logistic regression analysis found that higher medication adherence, good control fasting glucose as statistical predictors of good glycemic control as shown in Table 5. Multiple logistic regression analysis also found that others variables were not significantly associated with good glycemic control.
Multiple logistic regression analysis found that higher medication adherence, good control fasting glucose as statistical predictors of good glycemic control as shown in Table 5. Multiple logistic regression analysis also found that others variables were not significantly associated with good glycemic control.
Table 6. Multivariate analysis of factors associated with glycemic control
 IV. DISCUSSION
IV. DISCUSSION
In present study, the average HbA1c was 9.1 ± 2.6%. The proportion of patients having poor glycaemic control was 76.0% following HbA1c ≥7.0% criteria and 75.0% following Fasting glucose criteria, and the mean MMAS-8 score was 6.1 ± 1.6 out of a score range of 0-8. There were 51.0% who reported optimal medication adherence (MMA-8 > 6). There is significant association between demographic variables (living area, occupation, educational level), biochemical marker (HbA1c, fasting glucose, dyslipidemia) with medication adherence following MMAS-8. Only higher medication adherence, good control fasting glucose as statistical predictors of good glycemic control.
Study in Nhan Dan Gia Dinh hospital using MMAS-8 shows that proportion of poor medication adherence is very high, 30.7%. Following Le Thi Huong Giang, only 78.1% of patients is adherence[1].
Recently, the systematic reviews of diabetes medication adherence reported that in prospective studies, many patients had poor adherence to oral diabetes regimens which ranged from 67 to 85% and the overall adherence rate was from 36 to 93% in patients[2], [8], [9].
The present study findings regarding the association of educational level and medication adherence was consistent with previous studies[15]. Higher educational background of the patients might be associated with their awareness and concern to adhere to medication; they may understand and benefit from physician’s recommendations about the importance of their medication.
Previous studies confirmed that better diabetes control was significantly dependent on the adherence to medication. It indicated that medication adherence was not the only factor that associated with glycemic control and diabetes knowledge was another important factor. MMAS score has been found to be predictors of HbA1C[15], [13], [3].
Meaning of the Study
The implications of the present study findings are clear. Firstly, MMAS-8 was associated with HbA1c control, and poor medication adherence (defined as having MMAS-8 score < 6) was associated with the increasing level of HbA1c (poor glycaemic control). The weak correlation with small magnitude of relationship between the MMAS-8 score and HbA1c level suggested that the MMAS-8 instrument should be applied with caution when predicting glycaemic control for diabetes patients in clinical practice. Also, this study evaluated other independent factors associated with poor glycaemic and poor medication adherence. We suggested that physicians and other healthcare practitioners should monitor the medication-taking behavior more closely among younger adults and those with little regular exercise.
Limitation
Firstly, origination of MMAS-8 is English. Therefore, there are some misunderstand while translating into Vietnamese. Secondly, study sample is very small, 192 patients, and limitation in hospital. The last, some factors such as insurance, marriage stage, income… are not cover in this study.
V. CONCLUSIONS
This study revealed that adherence is among the modifiable factors that are associated with better glycemic control. Living area, occupation, educational level, HbA1c, fasting glucose, dyslipidemia relate with medication adherence following MMAS-8. Higher medication adherence, good control fasting glucose as statistical predictors of good glycemic control.
REFERENCES
- Khoa Dược, Bệnh viện Nhân Dân Gia Định (12/2013), “Khảo sát và đánh giá việc tuân thủ điều trị trên bệnh nhân đái tháo đường type 2 điều trị ngoại trú tại Khoa khám bệnh – Bệnh viện Nhân Dân Gia Định”, tr. 36.
- Abebe S. M., Berhane Y., A. Worku (2014), “Barriers to diabetes medication adherence in North West Ethiopia”, Springerplus, 3, pp. 195.
- Al-Qazaz H. Kh, S. A. Sulaiman, M. A. Hassali, et al (2011), “Diabetes knowledge, medication adherence and glycemic control among patients with type 2 diabetes”, Int J Clin Pharm, 33 (6), pp. 1028-1035.
- American Diabetes Association (2010), “Standards of Medical Care in Diabetes”, Diabetes Care 2010, 33 supplement 1, pp. 11-61.
- American Diabetes Association (2015), “Standards of Medical Care in Diabetes”, Diabetes Care 2015, 38 supplement 1, pp. 8.
- Brown Marie T., Bussell Jennifer K. (2011), Medication adherence: WHO cares? Mayo Clinic Proceedings,
- Centers for Disease Control and Prevention (March 2013), Medication Adherence
- S., C.J. Cohen-Stavi, M. Leibowitz, et al (2014), “Defining the role of medication adherence in poor glycemic control among a general adult population with diabetes”, PLoS One, 9 (9), pp. 108145.
- , AdamsA. S., C. M. Trinacty, et al (2007), “Relationship between patient medication adherence and subsequent clinical inertia in type 2 diabetes glycemic management”, Diabetes Care, 30 (4), pp. 807-812.
- International Diabetes Federation (2014), “IDF Diabetes Atlas update poster, 6th edn”, Brussels, Belgium: International Diabetes Federation, 2014., pp. 2.
- Morisky Donald E., Lawrence W. Green, David M Levine (1986), “Concurrent and predictive validity of a self-reported measure of medication adherence”, Medical care, 24 (1), pp. 67 – 74.
- Morisky Donald E., M. Robin DiMatteo (2011), “Improving the measurement of self-reported medication nonadherence: Response to Authors”, Journal of clinical epidemiology, 64 (3), pp. 255-263.
- U., M. A. Hassali, F. Saleem, et al (2016), “Disease related knowledge, medication adherence and glycaemic control among patients with type 2 diabetes mellitus in Pakistan”, Prim Care Diabetes, 10 (2), pp. 136-141.
- K., W. Slocum, D. C. Ziemer, et al (2005), “Patient adherence improves glycemic control”, Diabetes Educ, 31 (2), pp. 240 – 250.
- C., WuC. H., H. H. Wang, et al (2015), “Association between the 8-item Morisky medication adherence scale (MMAS-8) score and glycaemic control among Chinese diabetes patients”, J Clin Pharmacol, 55 (3), pp. 279-287.
 Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam
Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam