PARAMETERS OF 24 HOURS AMBULATORY BLOOD PRESSURE MONITORING IN TYPE 2 DIABETIC PATIENTS WITH HYPERTENSION
Nguyen Ta Dong, Tran Van Trong, Nguyen Dinh Dat
Cardiovascular Center – Hue Central Hospital
Abstract
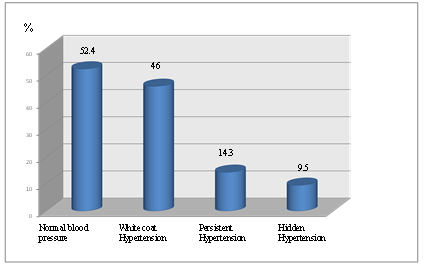
Objectives: Survey changes of blood pressure parameters in day and night, help to well control of hypertension in patients with type 2 diabetes. Subjects and methods: 63 type 2 diabetes patients, which is divided into two groups: Group with hypertension (SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg HATTrg) and group without hypertensive (SBP <140 and/or DBP < 90 mmHg), Methods: cross-sectional descriptive study. Results: Percentage of deeper blood pressure was 57.1%, non-deeper blood pressure was 42.9% at night. Rate overload of SBP, diastolic blood pressure during the day and night; rate of morning blood pressure rising in diabetic group with hypertension higher than diabetic group without hypertensive. The rate of “white coat” hypertension of subjects was 46%, hidden hypertension was 9.5%, persistent hypertension was 14.3%, normal blood pressure was 52.4%. Conclusions: The parameters on 24 hours blood pressure Monitoring in diabetic patients with hypertension were more disadvantaged than in group without hypertension.
Keywords: 24 hours ambulatory blood pressure monitoring (ABPM),Hypertension, type 2 diabetes
Main correspondence: Nguyen Ta Dong
Submission date: 1st August 2018
Revised date: 18th August 2018
Acceptance date: 31th August 2018
1.INTRODUCTION
At the present time, endocrine and metabolic diseases including diabetes are rapidly increasing, and are becoming an urgent problem for all of humanity. Type 2 diabetes is a multiform disorder, involving many tissues and organs in the body, especially the cardiovascular system. Compared with people without diabetes, hypertension is often twice as high in people with diabetes. Cardiovascular risk factors in which hypertension causes diabetes mellitus to have a higher risk of mortality and are more likely to be affected by diabetic cardiovascular automatic neuropathy, to develop complex progression[ ]. Measuring 24-hour ambulatory blood pressure monitoring is very important, allowing to provide parameters related to the disease. From that, we chosed the topic “Research on parameters of 24-hour ambulatory blood pressure in patients with type 2 diabetes with hypertension” with aimed at investigation of variability in blood pressure parameters in day and night helps us to classify hypertensives in patients with type 2 diabetes.
2. SUBJECTS AND METHODS
2.1. Subjects: Included of 63 patients diagnosed with type 2 diabetes, hospitalized in Medical Cardiovascular and Endocrinology – Neurology – Respiratory Department of Hue Central Hospital from August 2014 – August 2015, divided into two group:
* Study group: 38 patients with type 2 diabetes who had hypertension (HA≥140 / 90mmHg) were identified by normal BP measurement or history as having hypertension (taking hypertensive drugs).
* Control group: 25 patients with type 2 diabetes mellitus without hypertension (BP <140 / 90mmHg), as determined by normal BP measurement.
– Diabetic standard: American Diabetes Association (ADA) 2014.
– Diagnostic criteria for type 2 diabetes: Based on WHO criterias (1998), suitable for Viet Nam conditions:
– Standard diagnosis of hypertension in patients with diabetes:
+ According to the American Diabetes Association (ADA) in 2014 and the recommendation of the Vietnam Heart Association, when systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥ 90 mmHg.
+ 24 hour ambulatory blood pressure monitoring: systolic blood pressure ≥125 mmHg and/or diastolic blood pressure ≥ 80 mmHg.
– Exclusion criteria:
+ Patients can not stop taking hypertensive drugs when carrying Holter.
+ Patients with other serious medical diseases.
2.2. Methods: Cross-sectional descriptive study with comparing.
Age (in years), Gender, Time to detect diabetes, Treatment of diabetes. Review on Holter HA:
+ High blood pressure: Clinical blood pressure ≥ 140/90 mmHg and daytime ABPM> 135/85 mmHg.
+ White coat hypertension: systolic or diastolic blood pressure> 140/90 mmHg and ABPM mean daily blood pressure <135/85 mmHg.
+ Dipper status when nighttime blood pressure drops by ≥10% compared to daytime rest. If <10% of the mean daily blood pressure is “non-dipper” [8].
+ Early morning BP surge: systolic and diastolic blood pressureat the first 2 hours after waking up increased by at least 20/15 mmHg from the lowest BP during sleep.
+ Blood Presureoveroverload: percentage of measurements have high blood pressure. Normal <25%.
2.3. Data processing:
Using SPSS 16.0 and Excel 2010
3. RESULTS
1.Clinical characteristics and duration of detection of diabetes in the subjects
Table 3.1. Clinical characteristicsin the subjects
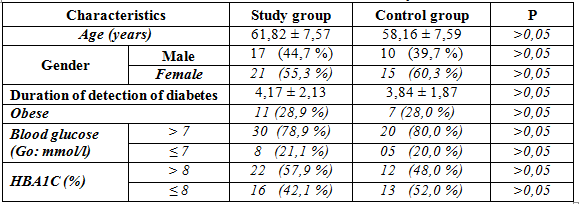 The group of diabetic patients with hypertension: male: 44.7%, female: 55.3%, non-hypertensive patients: male: 32%, female: 68%.
The group of diabetic patients with hypertension: male: 44.7%, female: 55.3%, non-hypertensive patients: male: 32%, female: 68%.
Table 3.2. Duration of detection of diabetes in the subjects
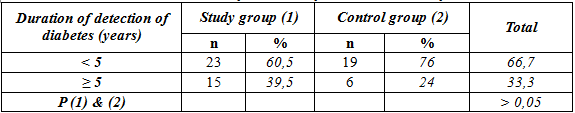 The group of diabetic patients with hypertension had difference was not statistically significantabout duration of detection of diabetes< 5 years and ≥ 5 years.
The group of diabetic patients with hypertension had difference was not statistically significantabout duration of detection of diabetes< 5 years and ≥ 5 years.
Table 3.3. Blood pressure and 24-housr heart rate in the subjects
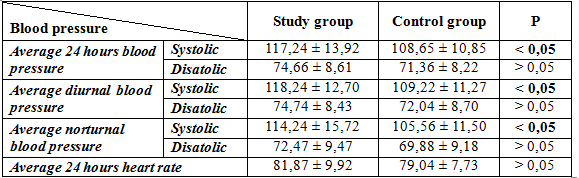 The difference of Average 24 hours blood pressure, Average diurnal blood pressure, Average norturnal blood pressure in diabetic patients with and without hypertension was significantly (p <0.05).
The difference of Average 24 hours blood pressure, Average diurnal blood pressure, Average norturnal blood pressure in diabetic patients with and without hypertension was significantly (p <0.05).
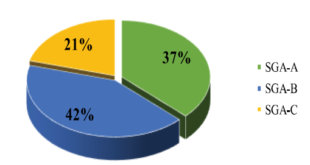
Chart 3.1. Types of hypertension in diabetic patients
Table 3.4. Dipper and non-dipper of norturnal blood pressure in the subjects
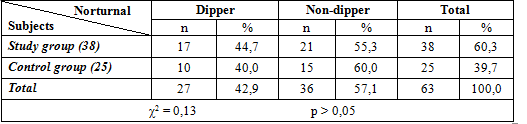 Difference of dipper and non – dipper norturnal blood pressure in diabetic patients with and without hypertension was not significantly (p >0,05).
Difference of dipper and non – dipper norturnal blood pressure in diabetic patients with and without hypertension was not significantly (p >0,05).
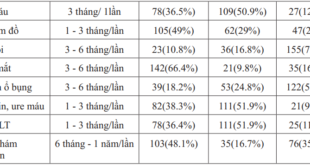
Table 3.5. Blood pressure over–overloading the subjects
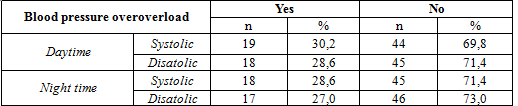 Table 3.6. Diurnal and norturnal blood pressure overload in the subjects
Table 3.6. Diurnal and norturnal blood pressure overload in the subjects
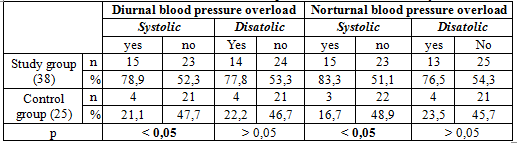 Daytime and nighttime blood pressure overload in diabetic patients with hypertension higher than non-hypertensive diabetic patients, statistically significant difference (p <0.05).
Daytime and nighttime blood pressure overload in diabetic patients with hypertension higher than non-hypertensive diabetic patients, statistically significant difference (p <0.05).
Table 3.7. Early morning blood pressure surge in the subjects
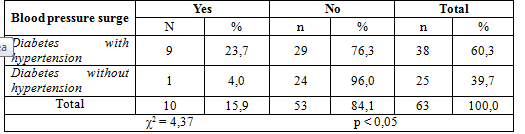 Percentage of early morning BP surge in diabetic subjects with hypertensionwas significantly higher than in non-hypertensive diabetic patients (23.7% vs. 4.0%, p <0.05).
Percentage of early morning BP surge in diabetic subjects with hypertensionwas significantly higher than in non-hypertensive diabetic patients (23.7% vs. 4.0%, p <0.05).
4. DISCUSSION
4.1. 24 Hours Blood Pressure variability of the study subjects.
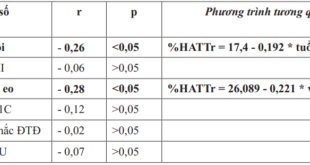
In our study results, blood pressure increased from 9 to 13 hours, the highest from 10 to 11 hours (121.17 mm Hg) and then decreased from 1.5 to 2.92 mm Hg from 13 to 15 hours. Blood pressure increased from 1.81 to 4.24 mmHg from 16-20 hours, the highest 17-18 hours (119.22 mmHg). Blood pressure decreases from 22 to 23 hours, the lowest in the day from 1-3 am. From 5 am, the HA gradually increases and starts a new cycle. Average 24-hour systolic blood pressure was 113.79 ± 13.40 mmHg, in which the diabetic group with hypertension of 117.24 ± 13.92 mmHg, the group of patients with non-hypertensive diabetes was 108.65 ± 10.85 mmHg. Average 24-hour diastolic blood pressure was 73.75 ± 8.55 mmHg, in which the diabetic group with hypertension 74.66 ± 8.61 mmHg, the group of non-hypertensive diabetic patients was 71.36 ± 8.22 mm Hg.
4.2. Blood pressure overload, early morning surge, dipper and non -dipper
* Blood pressure overload:
Prevalence of blood pressure overload was associated with the prognosis of hypertension specifically to cardiovascular events in hypertensive patients such as left ventricular hypertrophy, kidney damage, eyes, and brain… According to K. Madin et al [9], cardiovascular prognostic factors consisted of seven factors, including blood pressure overload.
According to Cao Chang et al [4], a 24-hour ambulatory blood pressure monitoring measurement of cerebral infarction with hypertension recorded elevated BP overload, almost BP increased during the day with non- dipper BP at night. The study of Ohkubo et al. [10] followed for 4.1 to 9.2 years of seeing cardiovascular mortality associated with 24-hour BP overload, increasing by 5% systolic BPor diurnal norturnal index of diastolic BP increases the risk of cardiovascular death by 20%.
The rate of systolic and diastolic blood pressure overload at day were 30.2% and 28.6%, respectively. The rate of systolic and diastolic blood pressure overload at night were 28.6% and 27,0 %, respectively.
In our study, prevalence of systolic and diastolic blood pressure overload at day in diabetic patients with hypertension was 78,9% và 77,8% respectivelyand higher than in diabetic patients without hypertension was 21,1% và 22,2%, respectively; prevalence of systolic and diastolic blood pressure overload at night in diabetic patients with hypertension was 83,3% và 76,5%, respectively and higher than in diabetic patients without hypertension was 16,7% và 23,5%, respectively. Difference systolic and diastolic blood pressure overload in diabetic patients with and without hypertension was significantly (p < 0,05).
* Early morning blood pressure surge
In this study, the prevalence of early moning blood pressure surge was 15.9%, in which hypertensive diabetes had 23.7%, non-hypertensive diabetes 4%, difference was significantly (p <0,05). According to Cao Tr Sinh et al. [4] in patients with cerebral infarction and hypertension, prevalence of early morning blood pressure surge was 57.9%. Early morning blood pressure surge is common in this population. In the majority of normal people, blood pressure variability with time of day, the highest at 17-18 hours, the lowest at midnight from 1 to 2 hours, from 2 am onwards blood pressure increased slightly in both systolic and diastolic blood pressure, Start increasing from 4 hours to daytime levels, in most cases increasing both systolic and diastolic blood prssure, at least 20/15 mmHg, and rarely >140/90 mmHg. A study by K. Madin et al. [9] in the UK found that 1187 subjects showed a early morning blood pressure surge of 47.07%. Compared with the two studies above, our prevalence of early morning blood pressure was lower, which may be due to different subjects and number of the patients.
* Dipper and non-dipper blood pressure:
The phenomenon of dipper or non-dipper blood pressure at night has been widely reported both domestically and internationnally. Huynh Van Minh et al [2] found that in normal subjects, the rate of dipper blood pressure at night was 56.7%, not dipper blood pressure was 43.3%; In men with hypertension these rates were 60% and 40%, the results showed that there was no difference between dipper and non-dipper BP in the same study subjects, no difference in the two rates between normal and hypertensive subjects. Cuspidi and colleagues [36] studied 36 type 2 diabetic patients with hypertension. The results showed that there were 11 patients with dipper blood pressure, (30.6%), and 21 non-dipper blood pressure patients (58.3%) and 4 patients with reversal blood pressure accounted for 11.1%. Our study showed that the prevalence of or dipper blood pressureat night in hypertensive diabetes was: 55.3%, non-hypertensive diabetes 60.0%. The percentage of non-dipper BP at night in the diabetic group with hypertension was 44.7%, and higher than the non-hypertensive diabetes group was 40.0%.
The difference dipper and non-dipper blood pressure at night between the two groups was not statistically significant (p> 0.05). The common finding in the study was that non-dipper BP at night in diabetic group with hypertension higher than non-hypertensive diabetes.
CONCLUSION
– The rate of nighttime dipper blood pressure was 57.1%, non-dipper blood pressure was 42.9%. (Group of diabetic patients with hypertension was 55.6%; in diabetic group without hypertension was 44.4%).
– The prevalence of systolic and diastolic blood pressure overload in diabetic patients with hypertension was higher than that innon-hypertensive diabetic patients.
– The prevalence of early morning blood pressure overload indiabetic patients with hypertension was 23.7%, and the non-hypertensive diabetic group was 4.0%.
– The white coat hypertension of the subjects was 46%, the hidden hypertension was 9.5%, the persistent hypertension was 14.3%, the normal blood pressure was 52.4%.
REFERENCES
- Lê Thanh Hải, Huỳnh Văn Minh (2008), “Tình trạng mất trũng huyết áp ban đêm xác định qua đo huyết áp lưu động 24 giờ và nguy cơ bệnh lý tim mạch”, Tạp chí Y học thực hành – Số 596, tr.306-316.
- Huỳnh Văn Minh, Cao Trường Sinh, Nguyễn Tá Đông (2015), Theo dõi huyết áp lưu động 24 giờ – Từ nguyên lý đến thực hành, Nhà xuất bản Đại Học Huế, tr.68-tr.240.
- Huỳnh Văn Minh (2014), Khuyến cáo của hội Tim Mạch Học Việt Nam về chẩn đoán, điều trị, dự phòng tăng huyết áp ở người lớn 2014, Hội nghị Tăng Huyết Áp Việt Nam lần thứ nhất 17-18/5/2014, pp1-54 .
- Cao Trường Sinh (2012), “Xác định hiện tượng mất trũng nhịp ngày đêm huyết áp ở bệnh nhân nhồi máu não giai đoạn cấp có tăng huyết áp bằng theo dõi huyết áp lưu động 24 giờ”, Y học Thực hành số 4/2014, tr.146-149.
- Lê Văn Tâm (2007), “Nghiên cứu tỷ lệ tổn thương một số cơ quan đích của tăng huyết áp ²Áo choàng trắng², bằng kĩ thuật đo huyết áp lưu động 24 giờ”. Luận văn thạc sỹ Y học chuyên ngành Nội khoa, trường Đại Học Y Dược Huế.
- ADA (2013), “Standard of Medical care in Diabetes”, Diabetes Care,Vol 36, pp.S13-S14, pp.S20-S21.
- Cuspidi C, Michev l, Meani S, Valerio C (2003), “Non-dipper treated hypertensive patients do not have increased cardiac structural alterations”, Cardiovascular Ultrasound, pp. 1-9.
- ESH/ESC (2013), “2013 ESH/ESC Guidline for the management of arterial hypertension”, European Heart Journal 2013, ESH and ESC Guidlines,pp. 56
- K, P. lqbal (2006), “Twenty four hour ambulatory blood pressure monitoring: a new tool for determining cardiovascular prognosis”, The Fellowship of Postgraduate Medicine, 82: 548-551.
- Metoki, Ohkubo, Kikuya M, Asayama K (2006),“Prognostic significance of night-time, early morning, and daytime blood pressures on the rick of cerebrovascular and cardiovascular mortality”, Journal of Hypertension, Vol 24 (9),pp.1841-1848.
 Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam
Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam