RELATIONSHIP BETWEEN LEVELS OF LIPID AND SLEEP QUALITY IN THE ELDERLY DIABETIC PATIENTS AT NATIONAL GERIATRIC HOSPITAL
Nguyen Thi Thu Huong1,2, Nguyen Thi Kim Chi2, Nguyen Trung Anh1,2
1 National Geriatric Hospital 2 Hanoi Medical University
DOI: 10.47122/vjde.2021.48.11
ABSTRACT
Background: Reduced sleep quality is common in advanced age. Poor sleep quality is associated with adverse outcomes, possibly because of its association with lipid disorder. However, the correlates of sleep quality in older populations are unknown. Objectives: To assess the association of levels of blood lipid with quality of sleep in older diabetic patients treated at National Geriatric Hospital. Methods: A cross-sectional study on 178 older diabetic patients treated at National Geriatric Hospital from March to October, 2020. Quality of sleep was assessed using the Pittsburgh Sleep Quality Index. Results: Among 178 participants, the mean age was 73.5 ± 8.0; female account for 57.3%. The rate of poor sleep quality was 67.4%. There was significant difference between cholesterol concentration and blood pressure ≥ 130/85 mmHg in female and sleep quality with p<0.05. There was no significant difference between fasting plasma glucose, triglyceride and HDL-C level, waist circumference and sleep quality. Conclusion: Our results confirm a high prevalence of poor sleep quality in older diabetic people. Early detection by performing PSQI for screening sleep disturbance in older diabetic patients then give appropriate treatment can help improved effectiveness of treatment as well as the patients’ quality of life.
Keywords: sleep quality, elderly, dyslipidemia, diabetes mellitus.
Main correspondence: Nguyen Trung Anh Submission date: 20th April 2021
Revised date: 26th April 2021 Acceptance date: 26th May 2021 Email: [email protected] Tel: 0903480774
1. INTRODUCTION
Sleep is one of the basic needs of human being and constitutes about one-third of human life and it’s very important and can impact every facet of our daily life. Poor sleep quality also affects health and well-being [1]. Generally, sleep disorders are common in the later life. A previous study among 240 older people at Geriatric National Hospital in 2019 shown that, prevalence of sleep disturbance in older people was 197 people (82.1%), while only 17.9% of participants (43 people) had good sleep [2].
Type 2 diabetes mellitus (DM) is a widespread metabolic disorder accounting for 95% of all diagnosed diabetes, which has affected approximately 190 million people around the world [3]. Several studies have acknowledged sleep disorder both in terms of sleep quality and quantity as an important risk factor for the incidence and progress of DM. Specifically in T2DM subjects, a cross- sectional study in 935 women demonstrated lower high-density lipoprotein (HDL) level in normotensive subjects with short and long sleep durations compared to mid-range sleep duration [4]. On the other hand, several studies have indicated that sleep duration and architecture are associated with obesity, diabetes, hypertension, cardiovascular disease, and in turn, with dyslipidemia [5],[6]. Several data indicate an association between the characteristics of sleep and the risk of cardiovascular events. For instance, the duration of sleep has been associated with left ventricular function and structure, while sleep disruption has been linked with atrial fibrillation. The quality of sleep maintains its prognostic value even in the oldest age. In fact, in oldest subjects a self-rated poor quality of sleep is associated with reduced survival [7], and an objective measure of sleep quality has been associated with physical performance [8]. Specifically, an association between poor sleep quality and dyslipidemia has been reported in younger and middle-aged adults; however, data are lacking regarding older populations [5],[6]. Thus, the aims of the present study were to assess the association, if any, of dyslipidemia with quality of sleep in older people.
2. SUBJECTS AND METHODS
2.1. Subjects
Older diabetic patients who were 60 years old and over, being examined and treated at National Geriatric Hospital from March to October, 2020. The patients have the physical and cognitive abilities to do a face-to-face interview. Exclusion criteria: patients had some conditions such as mental disorder; severe cognitive impairment or patients were inability to communicate.
2.2. Study design: the study was a cross- sectional study with convenience The sample size was calculated using the formula. From the formula, minimum sample size is 170 diabetic patients. Finally, the number of patients in our study was 178.
2.3. Variables
- General information: age, gender, weight, height, body mass index (BMI), blood pressure, smoking, drink
- Quality of sleep was assessed using the Pittsburgh Sleep Quality Index (PSQI) [9]:
The PSQI differentiates “poor” from “good” sleep by measuring seven domains: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, and sleep disturbances, use of sleep medication, and daytime dysfunction over the last month. The client self-rates each of these seven areas of sleep. The PSQI score is calculated by total points of seven components. Maximum of a normal sleep is less than 9. If result is more than or equal 9, the participant will get poor sleep.
- Blood tests: intravenous fasting blood was collected in the Fasting blood glucose, levels of lipid (cholesterol, triglyceride, LDL- C, HDL-C) were analyze.
2.4. Tools and data collection method
Data were collected by using research questionnaire through interview, diagnosis test, laboratory test and medical record at National Geriatric Hospital.
2.5. Data processing and data analysis
The process of data coding, entry into Redcap and analysis was done by using Statistical Package for Social Science (SPSS) software (version 20). Descriptive statistics were adopted to examine characteristic data: frequency, percentage, mean. Inferential statistics was done to perform comparisons between groups: t-Test Chi-square. Statistical significance was accepted at the 95% confidence level (p<0.05).
3. RESULTS
3.1. General characteristics
Table 3.1. Patient’s characteristics (n=178)
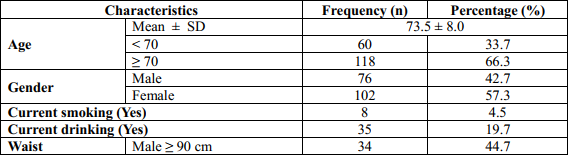
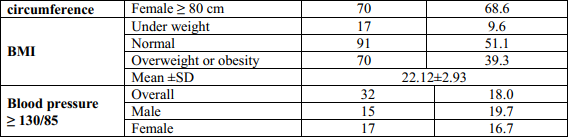
The mean aged of participants was 73.5 years old (SD=8.0) and the group of above or equal 70 years old was majority (66.3%). Almost participants was female (57.3%). The percentage of patients had current smoking and current drinking was very small, 4.5% and 19.7%, respectively. The mean of patient’s BMI was 22.12 kg/m2 and half of them had normal status (51.1%). The mean of waist circumference in male and female were 86.86 ± 15.41 and 83.78 ± 9.63, respectively. In the group of male patients, the prevalence of patients had blood pressure ≥ 130/85 mmHg was 19.7% and this rate in the female group was 16.7%.
3.2. The prevalence of sleep disturbance in study population
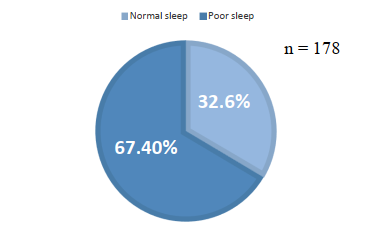
Figure 1. The prevalence of sleep disturbance in older diabetic patients
According to the PSQI scale, there were 120 participants (67.4%) had poor sleep, while only 58 participants (32.6%) had normal sleep.
3.3. Association between factors of levels of lipid and other factors and sleep quality
Table 2. Association between factors of levels of lipid and other factors and sleep quality
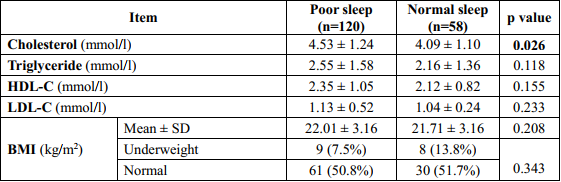
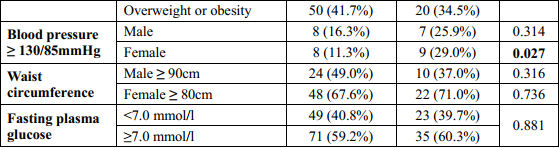
There was significant difference between cholesterol concentration and blood pressure ≥ 130/85 mmHg in female and sleep quality with p=0.026 and p=0.027, respectively. Patients with poor sleep had the mean of cholesterol concentration higher than patients with normal sleep (4.53 ± 1.24 and 4.09 ± 1.10, respectively). There were no statistical significance difference between other factors of metabolic syndrome and sleep quality, p>0.05.
4. DISCUSSION
In this study, we identified that prevalence of poor sleep quality in older diabetic patients was 64.7% with sleep quality cut-off by PSQI scale was 9 points. It was similar with research in 585 type 2 diabetic patients in Turkey, according to the PSQI, 64.3% experienced poor-quality sleep [10]. But this prevalence is higher than prevalence in research of 220 T2D patients in China, 47.1% [11]. The mean of PSQI scale was 10.63 ± 4.27 points, it was higher than the mean of PSQI in previous study in China, 8.3 ± 4.12 [11]; and higher than study in Turkey also, 6.18 ± 3.42 points [10]. The difference in result between studies can be explained by research subjects in this study was type 2 diabetic older patients (range of age from 60 to 96 years old), thus, quality of sleep was influenced by many factors: age, comorbid diseases and geriatric syndromes.
In this study, there were no significant difference between these two group of sleep quality of three lipidemia indexes (triglyceride, HDL-C and LDL-C), p>0.05. But, patients with poor sleep quality had an average cholesterol concentration of 4.53 ± 1.24 which was significantly higher than of the patients with good sleep quality, p=0.026. It was similar to the study of Barikani A (2019), which recorded that patients with short sleep duration had higher total cholesteron level compared with long/medium sleep duration groups [12]. This result was difference with result in previous research in China, there were no statistical difference between two group of sleep quality and lipidemia indexes [11]. Our study showed that there was no significant association between quality of sleep and fasting glucose control (p=0.881>0.05). It was the same fines in previous study in China, no significant association between sleep quality and blood glucose monitoring [11].
There were no statistical significance association between BMI and quality of sleep. A previous study in India among 202 patients with type 2 diabetes was the same result with p=0.371 [13]. Research in Poland was published in 2020 among 160 type 2 diabetic patients with median age of 69.50 years shown opposite result, which was significant association between BMI and quality of sleep with p=0.006 [14]. The difference in result can be explained by the difference with sample size, mean of age and cross-sectional study. This study shown that there were no statistically significant association between waist circumference and quality of sleep, p>0.05. It contrasted with previous research in Korea in 2018 which shown that there were statistically significant between waist circumference in male and female and quality of sleep, p<0.001 [15]. This difference can be explained by the sample size in this study was smaller than study in Korea (178 < 133,608), research subject and the mean of age.
This study considered that there was no statistically significant association between blood pressure ≥ 130/85 mmHg and quality of sleep in male, p>0.05. In contrast, there was significant association between blood pressure ≥ 130/85 mmHg in female, p=0.027. A research among 133,608 participants with mean of age was 53.6 ± 8.4 years old in Korea in 2018 shown that there were statistically significant between blood pressure ≥ 130/85 mmHg and quality of sleep in both male and female [15]. The difference between two studies can be explained by sample size in this study was smaller than sample size in Korean research and research subject. However, this result was similar to other studies around the world that demonstrated a link between sleep disorders and hypertension [16],[17].
5. CONCLUSIONS
Our results confirm a high prevalence of poor sleep quality in older diabetic patients. Cholesterol level and blood pressure had association with sleep quality. Early detection by performing PSQI for screening sleep disturbance in older diabetic patients then give appropriate treatment can help improved effectiveness of treatment as well as the patients’ quality of life.
REFERENCES
- Lee J.A., Sunwoo S., Kim Y.S., et al. (2016). “The Effect of Sleep Quality on the Development of Type 2 Diabetes in Primary Care Patients”, J Korean Med Sci, 31(2), 240–246.
- Hong Dao N.T, (2019). “The quality and pattern of sleep and related factors in older ipatients”, Hanoi Medical
- American Diabetes Association, (2010). “Diagnosis and classification of diabetes mellitus”. Diabetes Care. 33 Suppl 1:S62- 9.
- C. J. Williams, F. B. Hu, S. R. Patel, and C. S. Mantzoros, (2007). “Sleep duration and snoring in relation to biomarkers of cardiovascular disease risk among women with type 2 diabetes,” Diabetes Care, vol. 30, no. 5, pp. 1233–1240,.
- Zohal M, Ghorbani A, Esmailzadehha N, Ziaee A, Mohammadi Z, (2017). “Association of sleep quality components and wake time with metabolic syndrome: the Qazvin Metabolic Diseases Study (QMDS)”, Iran. Diabetes Metab Syndr. 2017.
- Lin S-C, Sun C-A, You S-L, Hwang L-C, Liang C-Y, Yang T, et al, (2016). “The link of self-reported insomnia symptoms and sleep duration with metabolic syndrome: a Chinese population-based study”, Sleep, 2016;39:1261–6.
- Qiu L, Sautter J, Liu Y, Gu D, (2011). “Age and gender differences in linkages of sleep with subsequent mortality and health among very old Chinese”. Sleep Med. 2011;12:1008–17.
- Kim M, Yoshida H, Sasai H, Kojima N, Kim H, (2015). “Association between objectively measured sleep quality and physical function among community- dwelling oldest old Japanese: a cross- sectional study”. Geriatr Gerontol Int. 2015;15:1040–8.
- Smyth C, (2003). “The Pittsburgh Sleep Quality Index. (Try This: Best Practices in Nursing Care to Older Adults from The Hartford Institute for Geriatric Nursing)”. MedSurg Nurs, 12(4), 261–263.
- Keskin A., Ünalacak M., Bilge U., et al. (2015). “Effects of Sleep Disorders on Hemoglobin A1c Levels in Type 2 Diabetic Patients”, Chin Med J (Engl), 128(24), 3292–3297.
- Zhu B.-Q., Li X.-M., Wang D., et al. (2014). “Sleep quality and its impact on glycaemic control in patients with type 2 diabetes mellitus”, Int J Nurs Sci, 1(3), 260–265.
- Barikani A, Javadi M, Rafiei S (2019). Sleep Quality and Blood Lipid Composition Among Patients with Diabetes. Int J Endocrinol Metab;17(3):e81062
- Sathyanarayanan A., Benny E., Osborn J., et al. (2015). “Factors Associated with Poor Sleep Quality among Type 2 Diabetes Mellitus Patients on Insulin Therapy”, J Diabetes Mellit, 05, 206–210.
- Mikołajczyk-Solińska , Śliwińska A., Kosmalski M., et al. (2020). “The Phenotype of Elderly Patients with Type 2 Diabetes Mellitus and Poor Sleep Quality”, Int J Environ Res Public Health, 17(16).
- Kim E., Shin S., Lee H.-W., et al. (2018). “Association between sleep duration and metabolic syndrome: a cross-sectional study”, BMC Public Health, 18(1), 720.
- Chiang GSH, Sim BLH, Lee JJM, Quah JHM (2018). Determinants of poor sleep quality in elderly patients with diabetes mellitus, hyperlipidemia and hypertension in Singapore. Prim Health Care Res Dev, 19(6):610-615.
- Nagai M, Hoshide S, Nishikawa M, et al. (2013). Sleep duration and insomnia in the elderly: associations with blood pressure variability and carotid artery remodeling. Am J Hypertens. 26(8):981-9.
 Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam
Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam