PREVALENCE AND CHARACTERISTICS OF DYSLIPIDEMIA IN PATIENTS WITH ACUTE CORONARY SYNDROME
Huynh Le Thai Bao 1,*
1Faculty of Medicine, Duy Tan University, Danang, Vietnam
DOI: 10.47122/vjde.2021.48.9
ABSTRACT
Objectives: Determining the prevalence and characteristics of dyslipidemia in patients with acute coronary syndrome at Central Highlands General Hospital from January 2019 to August 2019. Methodology: Using descriptive cross section method with convenience sampling method. Research on 216 patients diagnosed with acute coronary syndrome. Patients were clinically examined, subclinical tested, and interviewed with a prepared questionnaire. Dyslipidemia is diagnosed by testing lipid parameters when there is one or more of the following disorders: Blood cholesterol > 5.2 mmol/L (200 mg/dL), Triglyceride > 1.7 mmol/L (150 mg/dL), LDL- cholesterol > 2.58 mmol/L (100 mg/dL), HDL- cholesterol < 1.03 mmol/L (40 mg/dL). Proceed to determine the rate and characteristics of dyslipidemia in patients with acute coronary syndrome. Results: The prevalence of dyslipidemia in patients with acute coronary syndrome treated at Central Highlands General Hospital from January 2019 to August 2019 was 70.83%. In particular, the ratios of disturbed lipid parameters were increased Cholesterol 18.98%, increased Triglyceride 32.41%, reduced HDL-C 36.57%, increased LDL-C 41.2%. There was a statistically significant difference between the dyslipidemia rate among the sexes: Male 78.42% and female 57.14% with p <0.01. There was a statistically significant difference between the incidence of dyslipidemia between the forms of acute coronary syndrome: Unstable angina pectoris 54.95%, non-ST segment myocardial infarction 70% and ST-segment myocardial infarction 88.24 with p <0.05.
Keywords: Acute coronary syndrome, dyslipidemia, cardiovascular risk factors.
Main Correspondence: Huynh Le Thai Bao
Submission date: 20th April 2021
Revised day: 26th April 2021
Acceptance date: 26th May 2021
Email:[email protected], [email protected]
Tel: 0888838539
1. INTRODUCTION
Acute coronary syndrome is a particularly dangerous syndrome with severe sequelae. This is one of the leading causes of death in developed countries. According to Benjamin et al. (2014), 1,339,000 people were hospitalized in the United States for acute coronary syndrome, including 957,000 diagnosed with acute myocardial infarction and 382,000 with unstable angina [9]. In Vietnam, acute coronary syndrome is also increasing along with socio-economic development, according to the Vietnam National Heart Institute, in 2007, the percentage of patients admitted to the Heart Institute for Heart Attack is 9.1% [3]. According to Nguyen Thi Hong Hue et al (2013) at Cho Ray Hospital in 2010, 7,421 patients were hospitalized for angina (1,538 acute coronary syndrome and 267 deaths) [2]. Dyslipidemia is an abnormal condition when one or more lipid parameters are disturbed (hypercholesterolemia, hypertriglyceridemia, increased LDL-C, decreased HDL-C…) [8]. There have been many studies in the world and in the country showing the independent relationship between dyslipidemia and cardiovascular events. However, in the Central Highlands in general and in Dak Lak province in particular, which is a place with unique natural, economic and social characteristics, there has not been much research on dyslipidemia in patients with acute coronary syndrome. So we implemented the project with the goals:
- To determine prevalence of dyslipidemia in patients with acute coronary
- Identify some characteristics of blood lipid parameters in patients with acute coronary
2. SUBJECTS AND RESEARCH METHODS
2.1. Research location and time: The Central Highlands General Hospital from January 2019 to August
2.2. Subjects of study: All patients admitted to the Central Highlands General Hospital were diagnosed with acute coronary syndrome between January 2019 and August 2019.
2.3. Methodology
2.3.1 Design: Using descriptive cross section method with convenience sampling method
2.3.2. Sample
Sample size: The sample size is calculated according to the main goal of the project to determine the rate of dyslipidemia in patients with acute coronary syndrome and is calculated by the formula of calculating the sample size to estimate a proportion in the population.
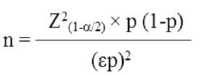
In which: n: Minimum sample size. α: Probability of type 1 error, if α = 0.05, Z (1-α / 2) = 1.96. p is the desired dyslipidemia rate, taken from the previous study of Pham Thi Thu Hong with p = 0.6512. Choose ε = 0.1, we calculate the sample size is n = 72. In fact, we have studied 216 patients, tripple that number.
2.3.3. Data collection
2.3.3.1. The main variables in the study
* Dyslipidemia: Diagnosis, determination of dyslipidemia according to NCEPATP III standards. Considered dyslipidemia when having one or more of the following disorders: Blood cholesterol> 5.2 mmol / L (200 mg / dL), Triglycerides> 1.7 mmol / L (150 mg / dL), LDL-cholesterol> 2.58 mmol / L (100 mg / dL), HDL-cholesterol <1.03 mmol / L (40 mg / dL) [6].
2.3.3.2. Measures to limit bias
Technical training for members of the investigation team. The questionnaires were tested and revised through trial research before conducting the official investigation. Face to face interview. Use measuring devices that meet design standards and the same type. Supervised during the investigation.
2.3.4. Processing and analyzing data
Enter and process data using SPSS software 20.0.199
– Descriptive statistics:
- Statistical analysis:
+ Compare dyslipidemia with some related factors by using the Chisquared test or Fisher’s exact test when there is> 20% expected frequency in the table <5.
+ The difference is statistically significant when p <0.05.
3. RESULTS AND DISCUSSION
+ Quantitative variables are described by mean and standard deviation.
3.1. General characteristics of the research sample
+ Qualitative variables are described by frequency and percentage. Table 1. Distribution of study subjects by age group and gender
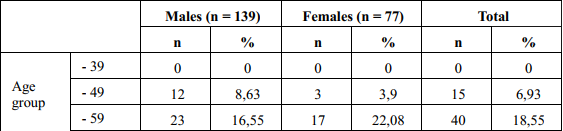
In our study, the gender ratio is: male 64.35% and female 35.65%, the male/female ratio is approximately 2 times; This result is similar to that of Do Thi Thu Ha et al. (2008) [5]: men accounted for 75.3% and women accounted for 24.7%, research by Pham Thi Thu Hong (2010) [7]. This is also consistent with many literature, and male gender is one of the cardiovascular risk factors. Regarding age group, the age group accounted for the highest proportion of 60-69 years old, accounting for 34.72%; This result is different from that of Pham Thi Huyen (2011) [5] with the highest age group of 70-79 years, accounting for 32.8%.
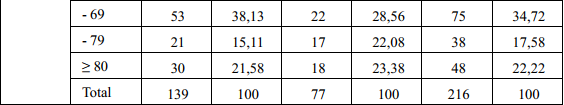
Table 2. Distribution of research subjects according to myocardial infarction type
Regarding the distribution of patients with acute coronary syndrome: ST segment myocardial infarction accounted for the highest proportion: 42.13%, followed by unstable angina: 39.35%, the lowest was non-ST segment myocardial infarction 18.52%; similarities with studies of Tran Nhu Hai and Truong Quang Binh at Cho Ray Hospital (2009) [9].
This result is different from that of Pham Thi Huyen at the general hospital in Dak Lak province (the precursor of the Central
Highlands General Hospital) (2011) [5] with unstable angina accounting for the highest rate was 50%, followed by ST-segment myocardial infarction: 34.3%, the lowest was non-ST segment myocardial infarction: 14.9%. This difference may be due to the introduction of the Interventional Cardiology Department (2016) with modern machinery systems, a team of highly skilled doctors resulting in advanced diagnosis and treatment of coronary syndrome, making the distribution of the disease similar to Cho Ray hospital.
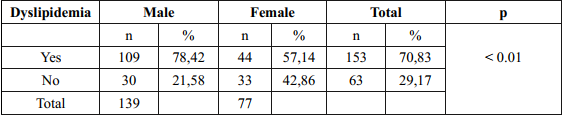
Table 3: The prevalence of dyslipidemia by genders
3.2. Prevalence and characteristics of dyslipidemia in patients with acute coronary syndrome
Table 4. Average values of lipid parameters of the study subjects
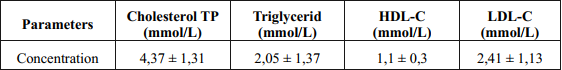
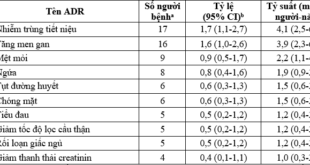
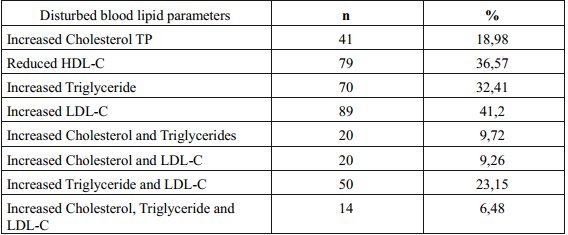
Table 5. The rate of disturbed blood lipid parameters of the study subjects
In our study, the prevalence of dyslipidemia was 70.83%, which is higher than that of Pham Thi Thu Hong at the hospital in Dak Lak province (2010) [7]: 65.12%. The prevalence of dyslipidemia in men is 78.42%, in women is 57.14%, this difference is statistically significant with p <0.01; This result is similar to the research of Pham Thi Thu Hong (2010) with the prevalence of dyslipidemia in men: 71.88%, female: 45.45% [7]. The prevalence of dyslipidemia in our study is higher than that of Pham Thi Thu Hong because it is possible that after 9 years, economic and social growth leads to an increase in many cardiovascular risk factors, including dyslipidemia.
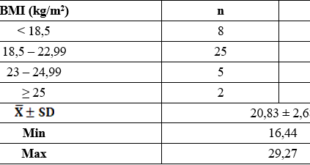
In our study, the average value of blood lipid parameters is Total Cholesterol: 4.37 ± 1.31 mmol / L, Triglyceride: 2.05 ± 1.37 mmol / L, HDL-C : 1.1 ± 0.3 mmol / L, HDL-C 1.1 ± 0.3 mmol / L, LDL-C 2.41 ± 1.13 mmol / L The rate of disturbed Lipid parameters was: increased Cholesterol TP: 18.98%, increased Triglyceride: 32.41%, decreased HDL-C: 36.57%, increased LDL-C 41.2%. This result is different from Pham Thi Thu Hong (2010) [6] with an increase in TP Cholesterol: 37.21%, Triglyceride: 16.28%, decreased HDL-C: 37.21%, an increase LDL-C 41.48%. This difference may be due to the difference in the sample size, Pham Thi Thu Hong’s sample size is 43, ours is 216 and due to the difference in the study time: 2010 and 2019.
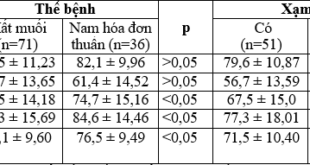
Table 6. Distribution of incidence of dyslipidemia according to acute coronary syndrome
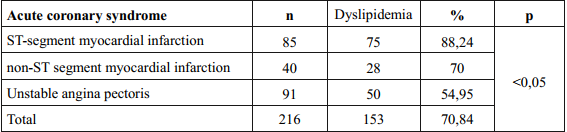
Table 7. Distribution of lipid disorders by place of some cardiovascular risk factors

In our study, the distribution of dyslipidemia by acute coronary syndrome was 88.24% for ST-segment myocardial infarction, non-ST segment myocardial infarction was 70%, Unstable angina pectoris was 70.84%, the difference was statistically significant with p <0.05. This result is consistent with many other studies in the world, including “Heart Disease and Stroke Statistics – 2018 Update” by Benjamin et al, (2018) [3], showing that the higher the prevalence of dyslipidemia, the more severe cardiovascular events.
Among cardiovascular risk factors such as smoking, hypertension, diabetes, in our study, the difference in the prevalence of dyslipidemia by type 2 diabetes was statistically significant: diabetes type 2 diabetes with dyslipidemia: 24.18%, type 2 diabetes without dyslipidemia: 14.29%, with p <0.05. This result is consistent with pathophysiology, in diabetes mellitus, when cells lack energy, lipids are mobilized, causing an increase in blood lipids [8].
4. CONCLUSION
- The prevalence of dyslipidemia in patients with acute coronary syndrome is 83%.
- Characteristics of dyslipidemia in patients with acute coronary syndrome:
+ The rate of dyslipidemia by gender is: male 64.35% and female 35.65% (p <0.01).
+ The average value of blood lipid parameters is: Total cholesterol: 4.37 ± 1.31 mmol / L, Triglyceride: 2.05 ± 1.37 mmol / L, HDL-C: 1.1 ± 0.3 mmol / L, HDL-C 1.1 ± 0.3 mmol / L, LDL-C 2.41 ± 1.13 mmol / L.
+ The rate of disturbed blood lipid parameters was: increased Cholesterol TP: 18.98%, increased Triglyceride: 32.41%, decreased HDL-C: 36.57%, increased LDL-C 41.2%.
+ There was a statistically significant difference between the incidence of dyslipidemia between the forms of acute coronary syndrome: Unstable angina pectoris 54.95%, non-ST segment myocardial infarction 70% and ST-segment myocardial infarction 88.24 with p <0.05
+ Distribution of dyslipidemia according to type 2 diabetes: type 2 diabetes [5] with dyslipidemia: 24.18%, type 2 diabetes without dyslipidemia: 14.29% (p <0.05)
REFERENCES
- Department of Immunology-Pathology, Hanoi Medical University, (2012), “Pathophysiology”, Medical Publishing House, 69.
- Do Thi Thu Ha et al, (2008), “Frequency and characteristics of metabolic syndrome in patients with coronary artery disease”, Ho Chi Minh City Medical Journal, vol. 12 No. 1, p. 43-49.
- Nguyen Lan Viet et al, (2007), “Study on the model of inpatient diseases treated at Vietnam Heart Institute during 2003- 2007”, Vietnam Journal of Cardiology, 52 , p.11-18.
- Nguyen Thi Hong Hue, (2013), “Study of NT-PRO-BNP values in short-term prognosis of non-ST elevation myocardial infarction”, Journal of Practical Medicine, No. 6/2013, 68-73.
- Pham Thi Huyen, Ngo Van Hung (2011), “Study on metabolic syndrome in acute coronary artery disease in general hospital in Dak Lak province”, Graduation thesis of GP in 2011, Faculty of Medicine Pharmacy, Tay Nguyen
- Pham Thi Thu Hong, Ngo Van Hung (2010), “Study on blood lipid index in patients with acute coronary artery syndrome”, Graduation thesis of GP in 2010, Faculty of Medicine and Pharmacy study the Central
- Tran Nhu Hai, Truong Quang Binh, (2009), “Characteristics of patients with acute coronary syndrome”, Ho Chi Minh City Medical Journal, vol 13, 1, pp.50- 55.
- ATP III (2001), Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III), Final Report.
- Benjamin et al, (2018), “Heart Disease and Stroke Statistics-2018 Update”, pp.337- 338.
 Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam
Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam