CLINICAL, SUBCLINICAL CHARACTERISTICS OF THYROID CANCER PATIENTS WERE TREATED BY ENDOSCOPIC SURGERY
Phan Hoang Hiep, Tran Ngoc Luong
Vietnam national hospital of endocrinology
DOI: 10.47122/vjde.2021.48.7
ABSTRACT
Background: Thyroid cancer accounts for 1% of all cancers. This is the most common type of malignant tumor affecting the endocrine system. The disease usually progresses slowly, mainly develops locally and metastases of neck lymph nodes. If detected early, it is possible to select appropriate treatment methods which will result in high efficiency. Objectives: To describe the clinical and subclinical characteristics of selected differentiated thyroid cancer patients in laparoscopic surgery. Methods: 115 thyroid cancer patients were performed endoscopic thyroidectomy at National Hospital of Endocrinology from March 2012 to April 2018. Results: 115 thyroid cancer patients were undergone endoscopic thyroidectomy at National Hospital of Endocrinology included 109 females (94.8%) and 6 males (5.2%). The proportion of female/male was 18/1. Age of patient were 15 to 45. Mean age of male was 30.4 ± 6.4 and 33.2 ± 4.5 of female. The most of nodules were not clear boundary (92.2%). 21.7% surface roughness, 80% nodules with solid density. 60/115 (52.18%) with metastatic neck lymph nodes, of which 61.7% central cavity lymph nodes; 38.3% bilateral metastatic neck lymph nodes. Papillary cancer accounted for 76.5%; 10.4% follicular, 13.1% papillary- follicular. Compared the results of FNA with pathology: 78.9% positive and false-negative rate was 7.8%. Conclusion: endoscopic thyroidectomy for thyroid cancer treatment is feasible, safe and cosmetic with selective cases.
Keywords: thyroid, cancer, endoscopy Main correspondence: Phan Hoang Hiep Submission date: 20th April 2021 Revised date: 26th April 2021 Acceptance date: 26th May 2021
Email: [email protected] Tel: 0904211839
1. INTRODUCTION
Thyroid cancer accounts for 1% of all cancers. This is the most common type of malignant tumor affecting the endocrine system [4], [7]. In histopathology, this tumor is divided into two subtypes: differentiated and undifferentiated. Clinical progress, treatment and prognosis of the two types are different. Differentiated cancer accounts for the majority of case (about 80%), including papillary, follicular and papillary-follicular.
The disease usually progresses slowly, mainly develops locally and metastases of neck lymph nodes. If detected early, it is possible to select appropriate treatment methods which will result in high efficiency [6], [7].
Research objectives are: Analyzing the clinical and subclinical characteristics of selected differentiated thyroid cancer patients in laparoscopic surgery.
2. SUBJECTS AND METHODOLOGY
2.1. Subjects
115 thyroid cancer patients were performed endoscopic thyroidectomy at National Hospital of Endocrinology from March 2012 to April 2018.
2.2. Selection criteria
Patients were diagnosis differentiated thyroid cancer with size of nodule <2cm, nodules were not invasive thyroid capsules,with/without metastatic lymph nodes were located by ultrasound, CT scanner, FNA under ultrasound guilded.
2.3.Exclusion criteria
Patients were diagnosis differentiated thyroid cancer with size of nodule >2cm, nodules cancer invaded thyroid capsules, strap muscles, trachea, easophagus, recurrent nerve.
Lymph nodes were Patients were history of head & neck surgery, history of head, neck, or upper mediastinal irradiation, inability to tolerate general anesthesia.
2.4. Study design
A prospective study was conducted
2.5. Data analysis
SPSS software 16.0 for medicine was used.
3. RESULTS AND DISCUSSION
3.1. Age and sex
According to a report by the American Endocrine Association (ATA 2015), differentiated thyroid cancer accounts for the majority, encountered at all ages, both men and women. Age and sex are associated with prognosis, people with age <15 or> 45 years of age are negative prognostic factors. The rate of women getting the disease is 2-3 times higher than that of men [1].
Table 1. Sex
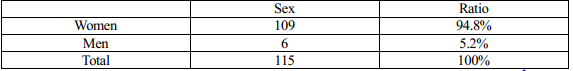
Table 2. Mean of age
![]()
In Vietnam, the studies of these authors showed that the percentage of female patients accounted for 2-3 times higher than that of men. Nguyen Tien Lang’s research has a significantly higher rate of women, 7.85 times compared to that of men. The common age group in the studies of Nguyen Quoc Bao and Tran Minh Duc is over 40 years old, in studies of other authors, the ages are from 31-45 years old.
Table 3. Sex ratio and average age of patients were treated by endoscopy
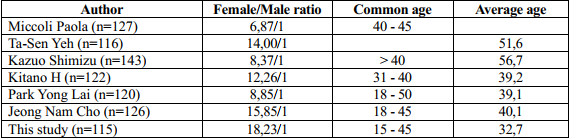
Patients selected in endoscopic surgery have a higher proportion of women, ranging from 6-18 times compared with men, depending on the author. This study has 115 patients with differentiated thyroid cancer, including 109 female patients (accounting for 94.8%) and 6 male patients (accounting for 5.2%). The lowest age is 15, the highest is 45, the average age of the patient is 32.7 ± 6.8, in which the average age of men is 30.4 ± 6.4 and that of women is 33.2 ± 4. , 5. The results of our research as well as domestic and foreign authors differ in the prevalence of common age groups and men/women ratio due to the difference in study subjects and scope … However, all of the studies show that the rate of differentiated thyroid cancer is quite widely distributed in terms of age, people of all ages can suffer from thyroid cancer, especially it is commonly seen in young people in working age. In all these studies, the average age of of thyroid cancer patients tend to be about 40, the working age, so the treatment to prolong the survival time for patients is very significant. Therefore, when a patient has a thyroid tumor, especially in the 40s, it is necessary to do tests to confirm thyroid cancer and apply early and thorough treatment for the patient to bring postivive result.
3.2. Funtional symptoms
Differentiated tumors are slow, quiet, and long- lasting. Initial symptoms are often scarce, difficult to detect, and have little diagnostic value. Symptoms such as choking, hoarseness, and a feeling of congestion in the neck are usually not the main symptoms for patients to check and treat. In the early stages of the disease, there are few specific symptoms that are valuable for early diagnosis, such as when patients who come to medical examination happen to find a thyroid tumor or cervical lymphoma, or there is a case of an enlarged tumor compressing neighboring organs. The appearance of unpleasant symptoms makes it easy to diagnose, but late illness affects treatment outcomes and disease prognosis [6], [8]. In our study: the first clinical symptom is also the reason for examination: patients with thyroid tumor: 21.8%, sore throat: 24.4%, discovered swallowing problems: 10.4% , choking 13.0% and hoarseness (1.7%). Patients who have hoarse throat were found to have vocal fibers and there ultrasound showed thyroid tumors. Research by Tran Minh Duc: 53.4% of patients with liver cancer have a feeling of pressure, entanglement, in the neck area; 38.9% choke when eating; 15.3% have hoarseness; 22.1% of local pain spread to the parotid [8]. According to Vu Trung Chinh: symptoms are quite scarce, most patients have average physiology; 4.8% of patients have weight-loss, these patients have had distant metastases or large tumors affecting normal activities. There is a low rate of l symptoms, poor body-wide symptoms; 98.8% of patients have no body-wide symptoms.
Patients who come to see a doctor can accidently discover a tumor or lymph node in the neck area, which partly helps diagnose the disease, but this is usually only in patients at a late stage, with tumor causing pressure or infection of surrounding organs such as: muscles, trachea, nerves. When thyroid cancer is detected and treated in a late stage, it is difficult for the surgeon to completely remove the thyroid gland and remove the cervical lymph nodes, due to the large size of the tumor and invaded nearby tissues, metastasis of many neck lymph nodes. Treatment results are limited, recurrence and metastasis rates are high.
3.3. Clinical signs
In the study we found that adenomas of the thyroid gland and neck lymph nodes are the 2 most common and the first clinical signs of thyroid cancer. Symptoms of hypothyroidism alone accounted for 35.7%, lymph nodes in the neck accounted for 13.9%, with both tumors and lymph nodes accounted for 38.3%. When having this symptom, the patient went to a specialist and discovered the disease. In clinical examination, we both found thyroid tumor in 100% of patients. However, while the rate of clinically detecting tumors in 2 lobes only 62.9%, the rate of case when thyroid ultrasound found tumors in both lobes increased to 85.2%. This proves that patients have many small tumors or tumors located deep in the parenchyma, in the posterior wall of the thyroid gland which could not be detected on examination. The rate of detection by ultrasound is 22.3% higher compared with clinical examination.
Table 4. Characteristics of the nucleus of the thyroid gland in the study group
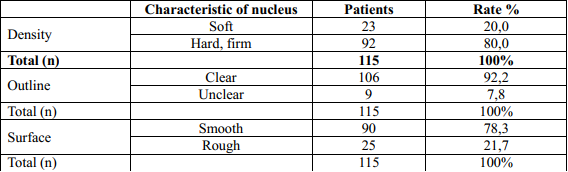
In this study, 80% of tumors have firm density and 20% of tumors have soft density. 78.3% of tumors have a smooth surface, 21.7% have a rough nucleus surface. According to Nguyen Tien Lang (2008), the thyroid nucleus appears individually or in association with the cervical lymph node in most patients, the symptom of pure thyroid gland is 54.8%; nucleus and nodule are 45.2. Research by Tran Trong Kiem (2008): 98.4% of patients have thyroid nucleus; 1.6% of patients do not have a thyroid nucleus but have a cervical lymph node. Aspirating these lymph node results in cervical lymph node metastasis, when the patient has thyroidectomy and cervical lymph node removal, it is observed that the nucleus has diameter <1 cm [13]. This shows that differentiated thyroid cancer progresses slowly and silently. Therefore, it is necessary to raise awareness about liver tumors so that people can understand and self-detect. When there is a thyroid tumor, it is necessary to examine and treat early to bring best results.
3.4. Ultrasound assessment of thyroid tumors: Many studies have published the ability to predict whether thyroid tumors are benign or malignant on the basis of ultrasonic Jin Joung Kwak et al (2011) gave a TIRADS classification based on 6 ultrasonic characteristics, including: Solid structure or predominant solid composition, hypoechoic, irregular margins or small zones, curvilinear calcifications, the height is greater than the width. The authors rated TIRADS from 1 to 6. In our study, the higher the TIRADS level, the greater the rate of cancer and similar to the numbers other authors reported: TIRADS 5: 63, 5%. TIRADS 4: 27.8 (TIRADS 4a: 4.4%; TIRADS 4b: 13.0%; TIRADS 4c: 10.4%). TIRADS 2 and 3 are only 1.7% and 7%.
Tumor size on ultrasound:
Our research results of endoscopic surgery: 84.3% of patients have tumors with size from 2–4cm, 15.7% of patients with tumors of 1 <u≤ 2 cm and tumors ≤ 1 cm in size 3 account for 5%. Hay et al. studied 1500 patients with papillary thyroid cancer. Patiens were monitored for 20 years, when the tumor was (2 – 3.9 cm), (4 – 6.9 cm) and the tumor was ≥ 7 cm. The corresponding mortality rates are 6%, 16% and 50%. Research of Kim BS et al (2014) papillary and follicular thyroid cancers, when the tumor size is less than 1.5 cm, and when the tumor is localized in the thyroid, it has almost not spread to the surrounding organization, it has hardly spread far. After 30 years, the recurrence rate was only 1/3 of that of the larger tumor, the mortality rate was 0.4% compared with 7% when the tumor size was ≥ 1.5 cm (p <0.01 ) [70].
Thus, when the tumor is small, the prognosis is better, after treatment, the rate of relapse and death is lower. Early examination when detecting neck tumors and subclinical coordination (ultrasound, radiology, CT …) to detect small thyroid tumors that are still deep in the thyroid parenchyma to increase efficiency better treatment and prognosis for the patient.
Number of tumors: According to the American Thyroid Association (ATA 2015), 50- 70% of thyroid cancer patients have 2 or more tumors. Clinical examination is difficult to detect small tumors or tumors located deep in the thyroid parenchyma, must be combined with ultrasound assessment and surgery [2]. According to Lee.J (2014), thyroid cancer is often abundant drive, after surgery 52% of patients have cancerous foci in both lobes, 30% have many small foci in one lobe, autopsy shows 25-36% of patients have microcarcinoma but conventional methods do not develop currently available. Our research: Thyroid ultrasound detects tumors that are not clinically visible, so the rate of thyroid tumors in the two lobes during ultrasound increases to 85.2% compared with clinical examination is 62.6 %. The number of 3 or more tumors accounts for 73%, patients with 2 tumors 25.2% and 1 tumor has 1.8%. Therefore, in diagnostic examination, it is necessary to be cautious, combine many subclinical methods to avoid missing small nuclei deep in the thyroid parenchyma that cannot be detected clinically.
Tumor margins: The margins of the tumor is an important factor in guiding the diagnosis and treatment. Thyroid tumors if the margins is not clear, the tumor surface is rough, and the density is firm towards thyroid cancer. In our research results, the boundary of the thyroid nucleus is determined on ultrasound. 92.2% of patients had ill-defined margins tumor with the remaining parenchyma, 7.8% had clear margins. In all patients the tumors have not yet invaded the surrounding organization. M. J and Cs (2015) studied 262 patients with papillary thyroid cancer, total thyroidectomy showed that the rate of invasion to the surrounding as: 53% muscle, trachea 37%, laryngeal nerve 47%, esophagus 21%, larynx 12% and invasions to other sites 30%. Ultrasound and CT scan of the neck are two tests that can determine the boundary of the tumor to the remaining glandular tissue and with the surrounding organization most quickly and conveniently [2].
* Ultrasound to evaluate neck lymph node metastases
Neck metastasis is a common symptom of thyroid cancer. Some patients came to the hospital because they found a cervical lymph node before the discovery of a thyroid nucleus. After clinical examination, ultrasound is the first test to detect whether there are lymph nodes or not, with the characteristics such as location, size, boundary, density … based on the criteria for suspecting cancerous lymph nodes from ultrasound image of ATA 2015 to evaluate each patient.
In our study, ultrasound has found nodes that cannot be detected by clinical examination (additional findings have lymph nodes increased by 25%). As a result, there were 60 patients with metastatic cervical lymph node, 42 patients were consider suspicious by ultrasound (accounting for 70%), 30% was not suspected. When compared with the results of CT scans with infused light-reflective drug, it showed that the suspected lymph nodes on CT (drug-infused lymph nodes) accounted for 73.3%, 3% higher than the suspected lymph nodes of ultrasound. Both of these methods had lower results towards detecting cancerous nodules than with fine-needle aspiration (78.3%). Thus, metastatic cervical lymph nodes of thyroid cancer can be detected by subclinical tests, each method has different sensitivity and specificity. It is necessary to coordinate the methods to guide the indication. and choose a suitable cervical ganglion dredging method.
3.5. Characteristics of cytology and histopathology
Cells aspiration with a fine-needle: Thyroid tumor cell aspiration for cytology diagnosis is the gold standard with many advantages: simple tool, fast, convenient results, high diagnostic value, less complications, can be done in many muscles Health service Dept. Cell aspiration need to be combined with ultrasound is very meaningful in diagnosis, especially when the thyroid tumor is small and deep, the test will give better results. Research of the American Thyroid Association (2015): fine-needle cells aspiration reachs a sensitivity of 79.54%; specificity is 96.7%; the accuracy is 88.7% and the positive forecast value is 95.5%. Comparing the results of the diagnosis of cytology and histopathology: the rate of positive results suitable for histopathology diagnosis is 65.9%, the rate of suspected diagnosis is 13.6%; the false negative rate is 20.5%. For papillary cancer the sensitivity is 81.2%; follicular is 61.6% [1].In this study, the rate of positive accounts for 87.9%, false negative accounts for 7.8%, and unspecified 4.3%. The results of our study have a higher rate of positive than other authors, but the accuracy of this method also depends on the tumor, the location of the puncture, the technique of taking samples and especially whether small tumors that are aspirated under the guidance of ultrasound or not. During surgery, if it is suspected that the lesion is cancer, then put the tumor organization cells on glass slides to get an accurate diagnosis and appropriate surgical methods.
Immediate biopsy: Peng Y.W. and Cs (2009) confirmed higher sensitivity and specificity of immediate biopsy than aspiration. The sensitivity of cell aspiration was 71%. The results of an immediate biopsy in surgery are more accurate than the aspiration test because the blood vessels and the penetration in the thyroid organization are visible. Immediate biopsy achieves sensitivity and specificity above 80%, and has important implications for surgical indications [3].
In this study, we put cell to glass slide in all cases, the positive rate accounts for 93.9%, false negative accounts for 2.7%, and suspicious cases accounts for 3.4%. This study result has a positive rate similar to that of other authors.
Table 5. Classification of histopathology of authors
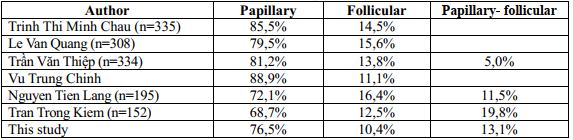
Histopathological classification: Currently, the histopathological classification of differentiated thyroid cancer including papillary, follicular and papillary- follicular tumors is used by the World Cancer Society and the American Cancer Society in clinical practice and research. Through studies, we found hat: in differentiated thyroid cancer, the rate of papillary cancer accounts for mainly from 68% – 88%. Follicular cancer accounts for 10% – 16%. Papillary-follicular thyroid cancer varies from author to author for the following reasons: authors can classify it as a separate category or by histopathological characteristics, it will be classified as either papillary or follicular.
– Nodules metastasis in the neck: is a common symptom of thyroid cancer. Some patients came to the hospital because they found that there were cervical lymph nodes even before the discovery of thyroid nucleus. At the time of diagnosis of thyroid cancer by puncturing at the nucleus or at the cervical lymph node, there were 5% of patients with papillary thyroid cancer, 10% of patients with follicular thyroid cancer or invasive Hurthle cells in the neck or distant metastases.
In our research group, there are 60 patients with cervical lymph node metastasis, accounting for 52.2% (table 3.21). The metastatic site is mainly found in the central cavity lymph nodes, accounting for 61.7%. Our study results are lower than that of Allanic H Slemen C (87%) but similar to other authors, showing that the metastatic lymph node encountered in the central cavity is the most common. This show that in the surgical procedure for thyroid cancer, the dredging of central cavity lymph nodes should be given priority. Lymph node metastasis on the same side with the tumor is 30%, the lymph node opposite to the tumor is 0%. When taking lymph nodes in each patient, we classified them into groups to do postoperative pathology. The results showed that the metastasis rate of the group VI lymph nodes was the highest, accounting for 35.8%. Group III, group IV and group V are similar, accounting for 18.4% respectively; 17.4% and 20.4%. The lowest metastasis in group I was 1.5%. Our research results are similar to those of domestic and foreign authors.
Relationship between lymph node metastases and histopathology: According to Shah D.H, Samuel A.M lymphoma metastasis in papillary cancer accounts for 42%, in follicular cancer it accounts for 17.2%. According to Fraker, neck lymph node metastasis in papillary cancer at the time of diagnosis accounts for 33 – 36%. Tran Van Thiep’s research shows that the rate of lymph node metastasis in papillary cancer is 78.3%. Vu Trung Chinh’s study showed that lymph node metastasis in papillary cancer accounted for 62.9%. In our study, papilloma metastatic lymphoma accounted for 59.1%, the rate of follicular lymph node metastasis is 25%, papillary-follicular lymph node metastasis is 33.3%. There is a difference in the lymph node metastasis between the histopathology with p <0.05. Compared with the study of foreign authors, the rate of lymph node metastasis in our study is lower, which can be because our chosen subject is in an early stage.
Cervical lymph node differentiated metastatic tumor is relatively high, all groups of cervical lymph nodes can metastasize. Tumor can combine with metastatic cervical lymph nodes or solitary metastatic cervical lymph nodes. Based on the frequency and location of metastatic cervical lymph nodes to guide the indication and choice of surgical removal of systemic or selective cervical lymph nodes.
4. CONCLUSION
Thyroid cancer is a common disease in many age groups, the most common age is 25-35 years old, accounting for 74.8%. Women are more vulnerable than men. A large proportion of patients have nucleus in both lobes. The characteristics of solid nucleus and unclear margin account for high percentages, which are 80%, 92.2% respectively. Aspiration is the best standard for diagnosis, while ultrasound helps to detect small nuclei that cannot be detected by clinical examination. Metastasis of cervical lymph node accounted for 52.18% rate, mainly group VI and lymph nodes on the same side with thyroid tumor. With differentiated thyroid cancer, the rate of papillary cancer accounts for mainly from 68% – 88%. Follicular cancer accounts for 10% – 16%.
REFERENCES
- Tran Minh Duc (2002). “Research, diagnostic and surgical treatment for thyroid cancer”, Doctor of Medicine thesis, Military Medical
- Tran Trong Kiem (2008). “A surgical research to remove the thyroid gland with radioactive iode 131I treatment of differentiated thyroid cancer”, Doctor of Medicine thesis, Military Medical
- Nguyen Tien Lang (2008). “Evaluate a combined total thyroidectomy 131I Treatment for differentiated thyroid cancer”, Graduate thesis of Specialist Doctor II, Hanoi Medical
- Tran Van Thiep, Phan Trieu Cung, Bui Xuan Truong and CS (2000). “Cervical lymph node metastasis of papillary thyroid carcinoma”, Ho Chi Minh City Medical Journal, 4, p. 148 – 203
- Karl B, David J.B, Clifford Y.K, Andren K.S et al (2012), “Extent of surgery affects survival for papillary thyroid cancer”, Annals of Surgery, 246 (3), pp. 375 – 380.
 Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam
Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam