INSULIN RESISTANCE IN HEART FAILURE PATIENTS
Tran Kim Son*, Nguyen Hai Thuy**, Huynh Van Minh**
(**) Professor. PhD. Hue University of Medicine and Pharmacy.
ABSTRACT
The study aimed to identify insulin resistance in heart failure patients with reduced ejection fraction (HFrEF) and preserved ejection fraction (HFpEF) and evaluate the significance of the HOMA index, QUICKI, I0, G0, I0/G0, I2/G2 in predicting the risk of insulin resistance in patients with HFpEF and HFrEF.
Subjects and methods:285 patients (114 patients with HFrEF (60%) and 76 patients with HFpEF (40%)) were studied, together with a control group of patients without heart failure (n=95). Blood insulin levels, blood glucose, HOMA index and QUICKI index of the participants were examined.Results:IR status was identified when HOMA index >2.53, QUICKI index < 0.33, I0>14.77, I2>107.95, I0/G0>3.81 or I2/G2>14.54.Based on HOMA index, the prevalences of insulin resistance in HfrEF and HRpEF groups were 58.8% and 50%, respectively, and they were significantly higher than the control group (p<0.001). The difference in insulin resistance between HFrEF and HFpEF patients was not statistically significant (p>0.05). Based on other indirect indexes including I0, G0, I0/G0, I2/G2 and QUICKI, the prevalences of insulin resistance and hyperinsulinemia in HFrEF and HFpEF groups were from 31.6% to 60.5% and from 26,3% to 50%, respectively. HOMA, QUICKI index and I0 were significant to identify the high risk of insulin resistance in HFrEF group (OR = 3.99, 3.49 (p <0.001) and 2.85 (p <0.01), respectively) and HrpEF group (OR = 2.8, OR = 3.49 (p <0.001) and 2.29 (p <0.01), respectively).Conclusion:Insulin resistance is present in patients with HFrEF and HFpEF. Indirect HOMA and QUICKI indexes can be applied to identify a very high risk of insulin resistance in patients HFrEF and HFpEF.
Keywords: Heart failure, Insulin resistance.
Main correspondence:Tran Kim Son
Submission date: 10 Feb 2017
Revised date: 22 Feb 2017
Acceptance date: 15Mar 2017
I. PROBLEM STATEMENT
Heart failure is a major burden on the community. The incidence of heart failure is rapidly increasing and the quality of life of patients with heart failure is lower than that of patients with other chronic diseases. Since the 1990s of 20th century, insulin resistance (IR) has been mentioned as a fundamental metabolic syndrome in several studies. Since 1998, the World Health Organization has launched diagnostic criteria for metabolic syndrome and IR [2]. Nowadays, the association between IR and heart failure is an interesting topic; however, the research on this issue is very scare [10], [11]. In Vietnam, there have been studies on IR in patients with hypertension, stroke, obesity, coronary heart disease in men, etc, but not in patients with chronic heart failure [1]. For the above reasons, it is urgent to carry out the study intitled “Insulin resistance in heart failure patients with reduced or preserved ejection fraction”.
The study aimed to explore the status and incidence of insulin resistance in heart failure patients with reduced and preserved ejection fraction and evaluate the significance of indirect indicators in predicting the risk of insulin resistance in heart failure patients with reduced and preserved ejection fraction.
II. SUBJECTS AND METHODS
2.1. Subjects
2.1.1. Selection criteria
Patients diagnosed with heart failure with heart failure according to the standards of 2012 European Society of Cardiology (ESC) and updated version in 2016 and hospitalised in Can Tho Central General Hospital from April, 2013 to May, 2016 were recruited.
2.1.2. Exclusion criteria
Due to potential effects on insulin sensitivity, patients with physiological and pathological status such as being pubertas, being pregnant, taking hormonal drugs (birth control pills, corticoid and cathecolamin), having diabetes or hypertension, BMI> 23 or waist circumference > 90 cm for men and > 80cm for women were excluded.
2.2. Methods
– A prospective cross-sectional study was applied.
– Sample size calculation:
n: Number of subjects, α: Significant level (0,05)
 p: Prevalence of IR in patients with chronic heart failure (0,53) [7]
p: Prevalence of IR in patients with chronic heart failure (0,53) [7]
d: Desired error 10% → d = 0,10
Therefore, the sample size is 95. To increase the accuracy, the sample size was doubled (n=190) and 95 patients without heart failure were selected in the control group.
-Patients with heart failure were diagnosed according to the standards of 2012 ESC, updated in 2016.
– Patients were classed as having HFrEF or HFpEF according to AHA/ACCF 2013, updated in 2016. HFrEF was defined by ejection fraction ≤ 40% and HFpEF by ejection fraction ≥ 50%.
– Methods for assessment of insulin resistance (according to WHO, 1999):
+ Assessment of insulin resistance by HOMA-IR index [2]
HOMA-IR = I0 x G0/22.55 (I0: Fasting blood insulin; G0: Fasting blood gluscose)
Cut-off value: the highest quartile of the control group
=> Normal HOMA-IR index <2.53.
+ Assessment of insulin resistance by QUICKI index
QUICKI= 1/log (I0 + G0)
Cut-off value: the lowest quartile of the control group.
=> Normal QUICKI index ≥0.33.
+ Assessment of insulin resistance by I0, G0, I0/G0, I2, G2, I2/G2 (I2:Insulin level two hours after meals; G2:Glucose level two hours after meals).
Select X+1SD of the control group.
– Ethical consideration:
+The proposal was accepted by the management board of Can Tho Central General Hospital and study subjects.
+ Information of study subjects was secured.
+ All subclinical costs were sponsored by the reseach funding.
– Statistical analysis:
Data were analyzed by using SPSS 22.0 software. Summary statistical methods (means, standard deviation and percentage) were employed. IR risk was evaluated by odd ratio.
III. RESULTS
The study sample comprised 285 patients (114 patients with HFrEF (60%) and 76 patients with HFpEF (40%)), together with a control group of patients without heart failure (n=95) hospitalised in Can Tho Central General Hospital from April, 2013 to May, 2016.
3.1 Status and prevalence of insulin resistance in patients with HFrEF and HFpEF
3.1.1 Insulin resistance
In this study, IR was evaluated by HOMA index: the highest quartile of the control group of 2.53 was applied (according to WHO). In addition, other indirect indexes were employed to evaluate IR such as:
– QUICKI index: the lowest quartile of the control group of 0.33 was used.
– I0, G0, I0/G0, I2/G2 indexes: select X +1SD of the control group:
I0 (9.44±5.29=14.77),
I2 (62.24±45.71=107.95),
I0/G0 (2.22±1.59=3.81),
I2/G2 (8.62±5.92=14.54).
3.1.2 Hyperinsulinemia
Hyperinsulinemia was diagnosed when I0> 14.77 (value of + 1SD of the control group)
Table 1:Distribution of IR and hyperinsulinemia by ejection fraction and indirect indexes
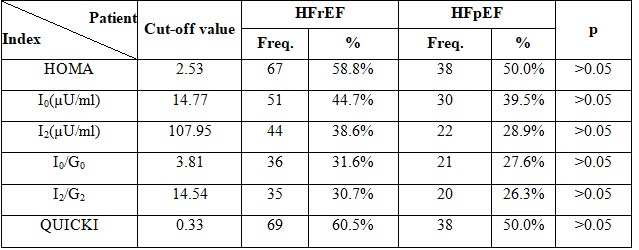 Remark: Based on HOMA index, QUICKI index, I0, I2, I0/G0 and I2/G2, prevalences of IR and hyperinsulinemia in patients with HFrEF were higher than in patients with HFpEF, but the differences were not statistically significant.
Remark: Based on HOMA index, QUICKI index, I0, I2, I0/G0 and I2/G2, prevalences of IR and hyperinsulinemia in patients with HFrEF were higher than in patients with HFpEF, but the differences were not statistically significant.
Table 2:Distribution of IR and hyperinsulinemia by groups and indirect indexes
(HOMA, I0, I2, I0/G0, I2/G2, QUICKI)
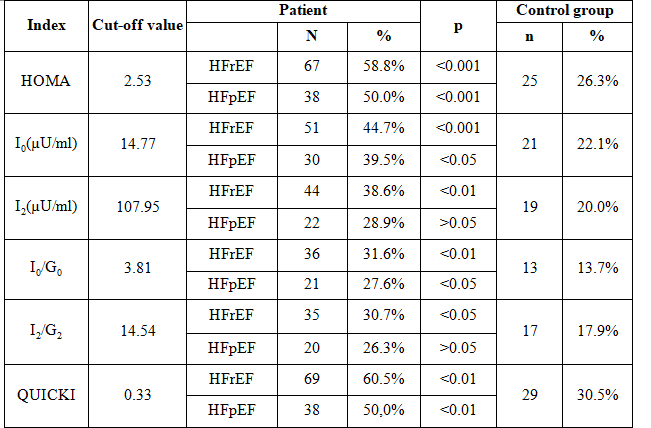 Remark: Based on HOMA index, QUICKI index, I0 and I0/G0, prevalences of IR and hyperinsulinemia in both patients with HFrEF and HFpEF were higher than in the control group (p <0,05).
Remark: Based on HOMA index, QUICKI index, I0 and I0/G0, prevalences of IR and hyperinsulinemia in both patients with HFrEF and HFpEF were higher than in the control group (p <0,05).
3.2 Evaluate the significane of indirect indexes in identifying the risk of IR in patients with HFrEF and HFpEF
3.2.1 Risk of IR in HFrEF group and control group
Table 3:Odd ratios of indirect indexes in HFrEF group and control group
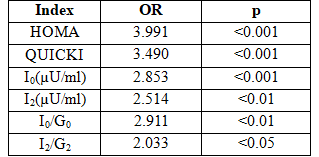 Remark: HOMA index, QUICKI index and I0 in the HFrEF group had high OR value (p <0.05).
Remark: HOMA index, QUICKI index and I0 in the HFrEF group had high OR value (p <0.05).
3.2.2 Risk of IR in HFpEF group and control group
Table 4: Odd ratios of indirect indexes in HFpEF group and control group
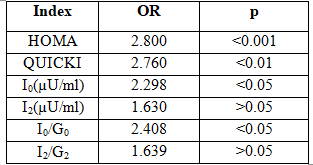 Remark: HOMA index in the HFpEF group had a very high OR (p <0.001). QUICKI index, I0 and I0/G0 in the HFpEF group had medium ORs (p <0.05).
Remark: HOMA index in the HFpEF group had a very high OR (p <0.001). QUICKI index, I0 and I0/G0 in the HFpEF group had medium ORs (p <0.05).
3.2.3 IR risk in HFrEF and HFpEF groups
Table 5: Odd ratios of indirect indexes in HFrEF and HFpEF groups
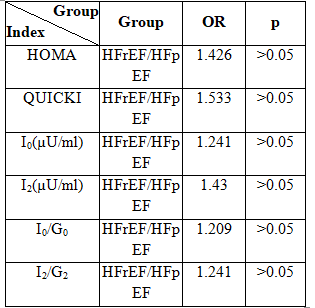 Remark: No statistical difference in IR risk was observed between HFrEF and HFpEF (p >0.05).
Remark: No statistical difference in IR risk was observed between HFrEF and HFpEF (p >0.05).
IV. DISCUSSION
4.1. Prevalences of IR and hyperinsulinemia in patients with HFrEF and HFpEF
The results of the study showed that prevalences of IR and hyperinsulinemia in bothHFrEF and HFpEF groups were higher than in the control group (p <0.05). Prevalences of IR and hyperinsulinemia in the HFrEF group were higher than in the HFpEF group, but the difference was not statistically significant at p> 0.05.
Based on the study of Funda Basyigit on identifying IR by HOMA-IR index on 50 heart failure patients without diabetes classified as NYHA I-III and aged 60 ± 10, prevalence of IR in the HFrEF group was higher than in the HFpEF group, but the difference was not statistically significant. In this study, patients with IR were defined by HOMA-IR index ≥2.7 (n=19) and patients without IR by HOMA-IR index <2.7 (n=31) [3]. The study result is consistent with our research finding. In HFrEF, humoral nervous is activated, which results in chronically reduced cardiac output leading to the increase in activation of the sympathetic nervous system and the RAA system. An increase in catecholamines reduced heart function with substrate metabolism, leading to an increase of circulating FFA level by stimulating lipolysis in fat cells [7].
This increases the concentration of circulating FFA and the activities of sympathetic system [10] and negatively affect to insulin signaling and reduce glucose utilization in skeletal muscle. The adverse metabolic effects of increased sympathetic system activity include inhibition of insulin secretion in pancreas and stimulating the gluconeogenesis and the glycogenolysis in liver, both of which increase the hyperglycaemia [3], [4].
4.2 Risk of IR in HFrEF and HFpEF
4.2.1 Risk of IR in HFrEF
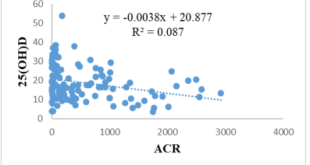
The study result revealed that indirect HOMA index, QUICKI and I0 determined a very high risk of IR in the HFrEF group compared with the control group with OR = 3.991, OR = 3.490, OR = 2.853, respectively (p <0.001). The remaining indirect indicators including I2 and I0 / G0 identified a high risk of IR in the HFrEF group with OR = 2.514 and OR = 2.911, respectively (p <0.05). I2 indirect indicator presented a moderate risk of IR in the HFrEF group with OR = 2.033 (p <0.05). According to the study of Wisniacki, the prevalence of HFrEF was 51% (n=27). When adjusted for age, BMI and Angiotensin Converting Enzyme inhibitors treating, heart failure patients had a very high risk of IR compared with the control group (OR = 0.88, 95% (CI) 0.70 to 1.11) [10]. IR is a risk factor in patients with chronic heart failure as it makes symptoms of heart failure worse and increases the mortality rate. In order to compare the differences in the risk of IR between HFrEF and HFpEF, Nadja Scherbakov carried out the study on 18 patients with HFrEF, 22 patients with HFpEF, 20 healthy people without diabetes and patients with clinically stable heart failure. IR was determined by indirect HOMA index and short intravenous insulin tolerance test. The study results showed a significantly negative correlation between the I0 concentration and the time period of short intravenous insulin tolerance test in the HFrEF group compared with the control group (y = 105-2x, r = -0 , 88, p <0.001) [5].
4.2.2 Risk of IR in HFpEF
The result of the study presented that risk of IR by indirect HOMA index is very high in the HFpEF group (compared with the control group) with OR = 2.800 and p <0.001. Indirect QUICKI and I0 were significant to identify IR risk in the HFpEF group with OR = 2.76, OR = 2.298, respectively (p <0.05). Indirect I2, I0/G0, I2/G2 indicators were not significant to measure the risk of IR in the HFpEF group.
The study of Wisniacki on 25 patients with HFpEF (accounting for 49%) showed that the HFrEF group had a very high risk of IR by indirect HOMA index compared with the control group (OR: 1.66, 95% CI: 1.35-2.03) [6]. The finding of this study is in keeping with our study that IR risk in the HFpEF group is higher than in the control group.This also shows that patients with HFpEF are at risk of IR at very early stage although it is very difficult for HFpEF to be clinically diagnosed. There is a left ventricular relaxation disorder in patients with HFpEF. Normally, this is a proactive process depending on beginning energy during the systolic ejection and continuing in equal volume relaxation and fast filling phases. In a normal heart, increasing in relaxation due to catecholamine when trying leads to the decrease in the pressure of left ventricular in the early diastolic phase.
Therefore, the relaxation is increased, which increases the pressure difference of left Atrial and left Ventricular, but not left atrial pressure and increases filled pressure when trying without increasing left atrial pressure. Cathecholamin increasing leads to a decrease of substrate metabolism and an increase of the blood FFA concentration, and then reduces insulin signaling and glucose utilization leading to IR risk in patients with HFpEF.
4.2.3 Comparison of IR risk between HFrEF and HFpEF
The study results presented that IR risk determined by HOMA index, QUICKI, I0, I2, I0/G0 and I2/G2 in the HFrEF group was higher than in the HFpEF group with OR = 1.426, OR = 1.533, OR = 1.241, OR = 1.543, OR = 1.209, OR = 1.241, respectively, but the difference was not statistically significant with p > 0.05. According to the research of Wisniacki on 25 people with HFrEF (49%), 27 people with HFpEF 51% STEFG, and a control group of 26 participants, HOMA index in the HFrEF group was higher than in the HFpEF group, but the difference of IR risk in two research groups was not statistically significant (0.88, 95% CI: 0 , 70-1.11) [6]. According to the study of Nadja Scherbakov, there was not a significant correlation between the I0 concentration and the time period of short intravenous insulin tolerance test in the HFrEF group compared with the HFpEF group and the difference of IR risk between HFrEF and HFpEF groups was not statistically significant [5]. The study is very consistent with our research. Although the prevalence of IR in the HFrEF group was higher than in the HFpEF group, the difference of IR risk between two groups was not statistically significant.
V. CONCLUSION
5.1 Insulin resistance was found in patients with HFrEF and HFpEF
– IR status was identified when HOMA index >2.53, QUICKI index < 0.33, I0>14.77, I2>107.95, I0/G0>3.81 or I2/G2>14.54.
-The prevalence of IR according to HOMA index
+ The prevalence of IR in the HFrEF group was 58.8% which is higher than in the control group (p <0.001)
+ The prevalence of IR in the HFpEF group was 50.0% which is higher than in the control group (p <0.001)
+ The difference of IR prevalences between HFrEF and HFpEF groups was not statistically significant (p >0.05).
– Prevalence of IR and hyperinsulinemia according to other indirect indicators including I0, G0, I0/G0, I2/G2 and QUICKI
+ Prevalence of IR in the HFrEF was from 31.6% to 60.5%.
+ Prevalence of IR in the HFpEF was from 26.3% to 50%.
5.2 Indirect indicators were significant to identify the risk of IR in HFrEF and HFpEF groups
– HOMA index was significant to predict a very high risk of IR in the HFrEF group (OR=3.99, p<0.001) and the HFpEF group (OR=2.8, p<0.001).
– QIUCKI index was significant to predict a very high risk of IR in the HFrEF group (OR=3.49, p<0.001) and a high risk of IR in the HFpEF group (OR=2.76, p<0.01).
– I0 index was significant to predict a very high risk of IR in the HFrEF group (OR=2.85, p<0.001) and a high risk of IR in the HFpEF group (OR=2.29, p<0.01).
REFERENCES
- Huynh Van Minh, 1996. Research on insulin resistance, a risk factor in patients with primary hypertension. Dissermination of PhD in Medical Science, Ha Noi.
- Nguyen Hai Thuy, 2008. Insulin resistance, Cardiovascular disease in endocrine and metabolic disorders. Hue University Publishing House, (9-58).
- Funda Basyigit and et al., 2010. The relationship between insulin resistance and left ventricular systolic and diastolic functions and functional capacity in patients with chronic heart failure and metabolic syndrome.Arch Turk Soc Cardiol,38, Issue: 3, pp173-181.
- MacDonald MR, Petrie MC, and et al. Hawkins NM, 2008. Diabetes, left ventricular systolic dysfunction, and chronic heart failure,Eur Heart J, 29: pp. 1224 –1240.
- Nadja Scherbakov, Maximiliane Bauer and et al., 2015. Insulin resistance in heart failure: differences between patients with reduced and preserved, left ventricular ejection fraction. European Journal of Heart Failure.
- N Wisniacki, W Taylor, et al., 2005. Insulin resistance and inflammatory activation in older patients with systolic and diastolic heart failure. Heart, 91: pp. 32-37.
- Patrick M. Heck, David P. Dutka., 2009. Insulin Resistance and Heart Failure. Cardiovascular Medicine, University of Cambridge, United Kingdom, 6(89-94).
- Tenenbaum A, Motro M, and et al. Fisman EZ, 2003. Functional class in patients with heart failure is associated with the development of diabetes,Am J Med, 114: pp. 271–275.
- Jonathan W.S, etc Stafan D.A., 1997. Insulin Resistance in Chronic Heart Failure: Relation to severity and etiology of heart failure. JACC, 30(2): pp. 527-532.
- Wilfried Dinh and et al., 2005. Insulin resistance and glycemic abnormalities are associated with deterioration of left ventricular diastolic function: a cross-sectional study. JACC, 46, (6), pp.0374-1097).
 Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam
Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam