SERUM HIGH SENSITIVITY C -REACTIVE PROTEIN (hs-CRP)
IN TYPE-2 DIABETIC PATIENTS
Nguyen Van Mui, Vu Bich Nga, Tran Hong Quang
ABSTRACT
Background: Elevated high-sensitivity C-reactive protein (hs-CRP) level has been shown tobe frequently associated with type 2 diabetes mellitus(T2DM); however, the related research in Vietnam has not been widely focused.Objective: to determineserum hs-CRP concentration intype 2 diabetic patients.Methods: A cross-sectional population-based study was done in 79type 2 diabetic patients and 46 nondiabetic subjects.Results:The mean serum hs-CRP concentration in diabetic group was 2.94± 2.14 mg/L and in normal healthy subjects was 1.68 ± 1.21 mg/L (p< 0.001). Serum hs-CRP level ≥ 3 mg/l was more statistically significantly frequent in T2DM group compared with nondiabetic one, 30.4% vs 6.5% (p<0.001), respectively.Conclusions:Serum hs-CRP level was significantly higher in the type 2 diabetic patients compared with nondiabetic ones (p<0.001). 54.4% of type 2 diabetic patients had serum hs-CRP levels between 1-3mg/L (a moderate risk for cardiovascular diseases) and 30 % had serum hs-CRP level > 3mg/L (a high risk for cardiovascular diseases).
Key word: serum hs-CRP, type 2 diabeticpatient
Main correspondence:Nguyen Van Mui
Submission date:8 Feb 2017
Revised date:20 Feb 2017
Acceptance date: 15Mar 2017
Introduction
Diabetes is a metabolic disorder with inappropriate hyperglycemia either due to an absolute or relative deficiency of insulin secretion or reduction in the biologic effectiveness of insulin or both. It is also associated with disturbances concerned with protein, carbohydrate and lipid metabolism [1].
Recent studies have suggested that low-grade chronic inflammation may be involved in the pathogenesis of type 2 diabetes [2], [3], [4], [5].
C-reactive protein, an acute-phase reactant produced by liver, is an extremely sensitive marker of systemic in-flammation. It is perceived that chronic low-grade inflammation as evidenced by elevated high sensitivity C-reactive pro-tein (hs-CRP) might potentially be a cause underlying the etiology andmanifestation of type 2 diabetes (T2D), although the exact mechanisms are still not well understood [6], [7].Additionally, hs- CRP has also emerged as a powerful predictor of cardiovascular disease (CVD) [8], [9], [10].
Vietnam is one of the Southeast Asia countries having the highest number of T2D individuals worldwide. However very few studies on hs-CRP have been done in type 2 diabetes patient.
Patients and Methods
Atotal of 125 subjects comprised of 79 diabetic patients as cases and 46 healthy individuals as controls were recruited from Endocrinology Department of Bachmai Hospital and Hanoi Medical University Hospital.
T2D was diagnosed in accordance with ADA 2012 criteria. Control subjects were recruited from the Health Check Department of Hanoi Medical University Hospitalwith normal fasting glucose (< 5.6 mmol/l) [16].
Type 1 diabetes patient, pregnant women, children, adolescents were excluded. All sujet with acute infectious or inflammatory disease or hs-CRP values greater than 10 mg/liter having be also excluded from analysis.
Plasma levels of hs-CRP were measured using Randox kit (HITACHI 717 machine).
Data for continuous variables are expressed as median and comparisonwith T-student test.
hs-CRP levels were classified into three categories, low risk(<1 mg/liter), intermediate risk (1–3 mg/liter), and high risk (>3mg/liter), according to the American Heart Association and Centersfor Disease Control recommendations [11].
Differences in distribution among the three categories were assessed using test.
Results
Table 1: Baseline characteristics of cases and controls
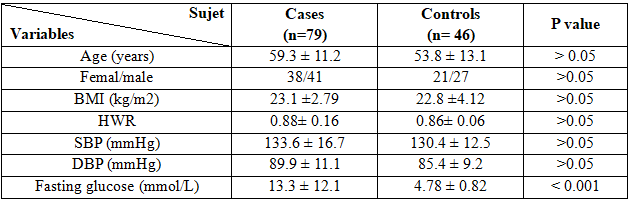 Body mass index (BMI); hip waist ratio (HWR); systolic blood pressure (SBP); diastolic blood pressure (DBP).
Body mass index (BMI); hip waist ratio (HWR); systolic blood pressure (SBP); diastolic blood pressure (DBP).
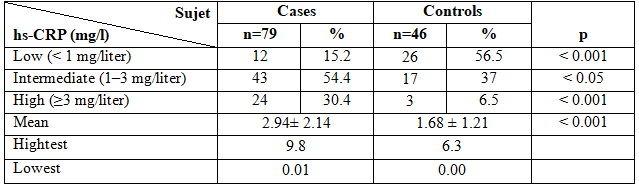
Table 2. hs-CRP level and their distribution in cases and controls group
 Discussion
Discussion
The purpose of this study was to assess the plasma hs-CRP level of type-2 diabetic patients and normal healthy people. Total of 125 subjects recruited, 79 cases and 46 controls.
The clinical and biochemical characteristics in relation to hs-CRP of the study group were shown on the table 1.
In comparison the characteristics between type 2 diabetes and non-diabetic subjects group, we observed no statistically significant difference about age, sex, BP, BMI, HWR.
The mean level of fasting blood sugar of the type 2 diabetes was 13.3 ± 12.1mmol/L,statistically significant higher as comparedwith the normal healthy group 4.78 ± 0.82mmol/L.
The hs-CRP level and their distribuation characteristics in T2Dand controls group were shown in table 2.
hs-CRP (mg/L) level of normal healthy people and diabetic patients were 2.94± 2.14 mg/L and 1.68 ± 1.21 mg/L respectively.The difference in the plasma hs-CRP level between normal people and type 2 diabetic patients are significant (P<0.001).
In a study by A.K.M. FAZLUL HAQUE et al. showed in 2010 that subjects with diabetes-2 had higher baseline levels of C-reactive protein, with normal healthy people [12].
Anubha Mah et al in the year 2009or Idrees Khan, Kauser Usman et al in 2012, showed that in comparison with normal control(healthy people) serum hs-CRP was significantly increased in type-2 diabetes mellitus group (P<0.001) [13], [14].
In a study in HongKong in 2003 by KATHRYN C.B. TAN et al showed that hs-CRP wasd significantly higher in T2D group than IGT group and thecontrol [6].
In our study mean hs-CRP level of healthy people were found 1.68 mg/L which was in mild risk for cardiovascular disease(<1mg/L).
Besides these inour study we have found that mean hs-CRP of type 2 diabetic patients was 2.94 mg/L which wassignificantly higher than that of the normal healthypeople (p<0.01)] and at limit of high risk for cardiovascular disease.
When study the hs-CRP level distribution, we classified into three categories. Subjects were characterised as high risk using hs-CRP cut off >3.0 mg/l, intermediate risk (1–3 mg/liter), low risk (< 1 mg/liter), according to the American Heart Association and Centers for Disease Control recommendations [11]. We observed that 43 diabets patients (54.4 %) had the hs-CRP concentration between 1-3 mg/l and 24 patients (30.4 %) had the hs-CRP level ≥ 3 mg/l; in the nondiabetic there was 56% of the subjets had the hs-CRP level under 1mg/L; only 6.5% (3 subjets) had hs-CRP level ≥ 3 mg/l (p< 0.001).
Kathryn C.B Tan, Nelson M.S, Sidney C.F. Tam et al, showed in 2003 when follow –up the hs-CRP level in 222 type 2 diabetic patients that 36.03% patients were in the high risk group for CVD (level of hs-CRP ≥ 3 mg/l) and 60.01% of type 2 diabetic patients in the intermediate risk group for CVD (hs-CRP level 1–3 mg/liter) [6].
Another study showed by Anubha Mahajan, Rubina Tabassum, Sreenivas Chavali in 2009 that: 66 % of type 2 diabetic patients had hs-CRP level between 1-3 mg/l, as intermediate risk for the CVD [13].
Consclusion
Median hs-CRP levels in the type 2 diabetes were 2.94± 2.14 mg/L, significantly higher compared to their nondiabetic counterparts (1.68± 1.21 mg/L).
The majority of type 2 diabetic patient (54.4 %) had hs-CRP level between 1-3mg/L (moderate risk for cardiovascular diseases) and 30 % of type 2 diabetes patients had hs-CRP levels> 3mg/L (high risk for cardiovascular diseases).
REFERENCES
- WHO (2011), “Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia”, report of a WHO/IDF consultation, 2006.
- Aldhahi W, Hamdy O “Adipokines, inflammation, and endothelium in diabetes. Curr Diab Rep 2003;3:293-98”, MedlineOrder article via Infotrieve
- Coulon J, Willems D, Dorchy H, “Increase in C-reactive protein plasma levels during diabetes in infants and young adults. Presse Med. 2005; 34: 89–93.
- Graziella Bruno et al (2009), “C-Reactive Protein and 5-Year Survival in Typ 2 Diabetes the Casale Monferrato Study”, Diabetes, vol 58, April 2009.
- Yves Mugabo (2010), “Régulation de la protéine C-réactive vasculaire dans le diabète de typ 2” Mémoire présenté à la Faculté des études supérieures en Nutrition, Université de Montréal.
- Kathryn C.B Tan, Nelson M.S, Sidney C.F. Tam, et al (2003) “C-Reactive Protein Predicts the Deterioration of Glycemia in Chinese Subjects with Impaired Glucose Tolerance”, Diabetes care, Volume 26, number 8, August 2003
- David M. Capuzzi et al (2007), “C – reactive protein and Cardiovascular Risk in the Metabolic Syndrome and Typ 2 Diabetes: Controversy and Challenge”, Volume 25, Number 1, 2007 16, CLINICAL DIABETES.
- Holman RR1, Paul SK, Bethel MA, Matthews DR, Neil HA (2008), “United Kingdom Prospective Diabetes Study (UKPDS): 10 years follow-up of intensive glucose control in typ 2 diabetes”,http://www.ncbi.nlm.nih.gov/pubmed/18784090
- Renu Virmani et al (2002), “Elevated CRP values and atherosclerosis in sudden coronary death”, Circulation, 105, pp. 2019-29.
- Paul E. Szmitko, Chao-Hung Wang et al (2003), “New markers of inflammation and endothelial cell activation”, “Biomarkers of vascular disease linking inflammation to endothelial activation”, Circulation,108, pp. 1917-27, 2041-51
- Centers for Disease Control and Prevention; American Heart Association (2003) “Markers of inflammation and cardiovascular disease: application to clinical and public health practice”, a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation 107:499–511
- K.M Fazlulhaque et al (2010), “Evaluation of serum High Sensitivity C- Reactive Protein in Typ 2 Diabetic Patient”, J MEDICINE 2010; 11: 20-23
- Anubha Mahajan, Rubina Tabassum et al (2009), “High-Sensitivity C-Reactive Protein Levels and Typ 2 Diabetes in Urban North Indians”, J Clin Endocrinol Metab, June 2009, 94(6): 2123–2127
- Idrees Khan, Kauser Usman et al (2012), “Association of Hs-CRP and HbA1C with Microalbuminuria in Type-2 Diabetic patients in North India”. Biomedical Research 2012; 23 (3):
380-384. - Safiullah Amanullah et al (2010), “Association of hs-CRP with Diabetic and Non-diabetic individuals”, Jordan Journal of Biological Sciences, Volume 3, Number 1, January 2010 ISSN: 1995-6673, Pages 7–12.
- International Diabetes Federation (2012), “Global Guideline for Typ 2 Diabetes”
- Syed Shahid HABIB, (2013), “Serum lipoprotein and high sensitivity C reactive protein levels in Saudi patients with typ 2 diabetes mellitus and their relationship with glycemic control”, Turkish Journal of Medical Sciences, (2013), 43: 333-338
 Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam
Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam