SKIN MANIFESTATIONS IN DIABETES MELLITUS: A CLINICAL STUDY
Nguyen Thi My Linh 1, Pham Thi Lan 2,3, Nguyen Khoa Dieu Van 1,3
1 Department of Endocrinology and Diabetes, Bach Mai Hospital
2 Hanoi Medical University
3National Hospital of Dermatology and Venereology
DOI: 10.47122/vjde.2022.53.6
ABSTRACT
Background: Skin diseases are among common injuries in diabetes. Skin changes play a role as an early manifestation as well as a
reflection of glucose metabolic control and chronic complication management of diabetes.
Objective: To evaluate clinical and laboratory features of diabetic patients with skin manifestations and the relation between common skin diseases and chronic diabetic related characteristics. Patient and method: 109 patients with type 1 and type 2 diabetes having skin injury hospitalized in Diabetic and Endocrinology Department of Bach Mai hospital and National Hospital of Dermatology from August 2019 to August 2020. Result: The prevalence of male and female patients in the study were 52,3% and 47,7% respectively, with the mean age of 60,46 ± 15,27. There were 4,6% patients with DM type 1 and 95,4% with DM type 2, the mean duration of DM was 7,71 ± 7,78 years. The most prevalent cutaneous findings were xerosis (59,6%), bacterial infection (22%), fungal infection (15,6%), onychodystrophy (19,3%), diabetic dermopathy (7,3%). The majority of patients (57,8%) had more than one type of skin injury. Of 109 patients, 33% had nephropathy, 27,5% had retinopathy, 29,8% had neuropathy; the prevalence of stroke, coronary artery disease and peripheral artery disease was 12,8%, 9,2% and 6,4% respectively. There was a statistically significant relationship between some common skin manifestations and duration of diabetes and microvascular complication, however, similar relation had not been found regarding such skin lesions and macrovascular diseases.
Conclusion: The most frequent cutaneous manifestation in patients with diabetes were xerosis, bacterial infection, fungal infection, onychodystrophy and diabetic dermopathy. Skin disorders may hint the existence of microvascular complication of diabetes.
Keyword: cutaneous manifestation, bacterial infection, fungal infection, xerosis, onychodystrophy, diabetic dermopathy.
Main correspondence: Nguyen Thi My Linh
Submission date: 19th Oct 2022
Revised date: 19th Nov 2022
Acceptance date: 19th Dec 2022
Email: [email protected]
Tel: + 84 234 943961968
1. INTRODUCTION
Diabetes is a global health challenge with rapid increase in incidence and on a large scale. Chronic hyperglycemia leads to many complications such as neuropathy, microvascular and macrovascular complication, affecting systematic organs including skin disorders [1]. Data from many different studies show that skin disease presents in 30 – 91.2% diabetic patients at a certain time of the disease course, with a variety of manifestations ranging from benign lesions, distortion, and even life-threatening conditions [2]. These manifestations can be early symptoms of metabolic disorders to help diagnose diabetes mellitus, on the other hand, they are also suggestive signs to prompt physicians to pay more attention to blood glucose control and chronic complications of diabetes. The detection of skin lesions plays an important role in improving the quality of life for diabetic patients, limiting the major complications of chronic hyperglycemia. In the world, there have been many published studies on diabetic dermopathy, however, there have been no studies in Vietnam revealing the rate of skin diseases and the relationship between cutaneous manifestations and chronic complications in patients with diabetes. Thus, we conducted this study.
2. SUBJECT AND RESEARCH METHOD
2.1. Subject: 109 inpatients with type 1 and type 2 diabetes at Department of Endocrinology and Diabetes, Bach Mai Hospital and National hospital of Dermatology and Venereology in one- year period, from August 2019 to August 2020.
2.2. Research method:
– Cross-sectional descriptive study.
– Record information about diabetes:
+ General and laboratory features of diabetes: Age and gender; disease duration; type of diabetes; BMI index; HbA1c concentration; glucose levels at admission; lipid levels (Cholesterol, Triglycerides, LDL-Cholesterol, HDL-Cholesterol); kidney function tests (blood creatinine, urine protein).
+ Macrovascular complication: Cerebrovascular accident, coronary artery disease, peripheral artery disease.
+ Microvascular complication: retinopathy, nephropathy, peripheral neuropathy.
– Skin lesions in diabetic patients: clinical examination and testing, if necessary, including direct fungal microscopy, bacterial culture test, and skin biopsies.
– The relationship between skin lesions and features of diabetes mellitus
+ Relation between common skin manifestations and disease duration, HbA1c concentration, retinopathy, peripheral neuropathy, nephropathy, macrovascular complication.
– Data processing using SPSS 25.0
3. RESULTS AND DISCUSSION
3.1. General features and pathological of diabetes mellitus
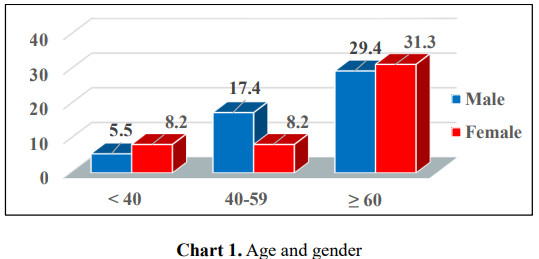
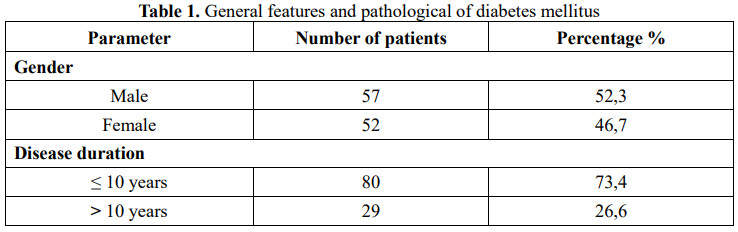
In our study on 109 diabetic patients with cutaneous manifestations, the average age was 60.46 years, ranging from 22 years old to 90 years old. In which, 60.6% of the patients was aged 60 or above, 57 male patients accounted for 52.3% and 52 female patients made up 46.7%. There was no difference between the genders. The average time of diabetes in this study was 7.71 ± 7.78 years. However, 25 patients (22.9%) were newly diagnosed. This result is remarkable since some patients were diagnosed with diabetes by detecting cutaneous manifestations. On the other hand, there were patients with a 35-year history of diabetes, this finding suggests that diabetic patients in Vietnam have been received better treatment in the recent years.
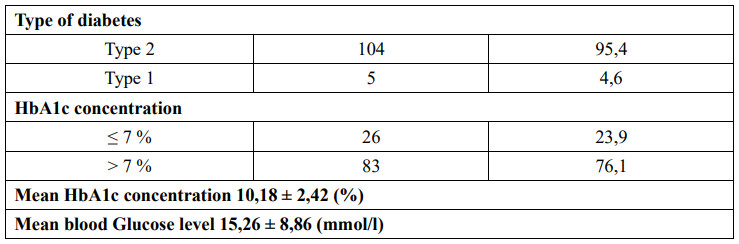
Most of the patients were type 2 diabetes, accounting for 95.4%. The mean HbA1c concentration was 10.18 ± 2.42 (%). The percentage of patients with HbA1c > 7% was 76.1% (83 patients). The mean blood glucose level at admission was 15.26 ± 8.86 mmol/l.
3.2. Diabetes complications
3.2.1. Macrovascular complication
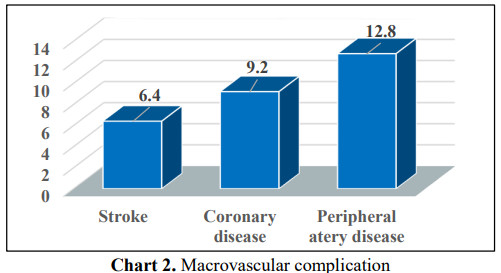
Macrovascular complication in diabetic patients is caused by atherosclerosis in medium and large vessels. In our study, the rate of patients with peripheral artery disease, coronary artery disease and cerebrovascular accident respectively was 12.8%; 9.2% and 6.4%. Other authors in the world also indicated different results. According to Duriye (2013) et al., up to 17.5% of patients had macrovascular complication including coronary artery disease, peripheral artery disease and cerebrovascular accident [3].
3.2.2. Microvascular complication
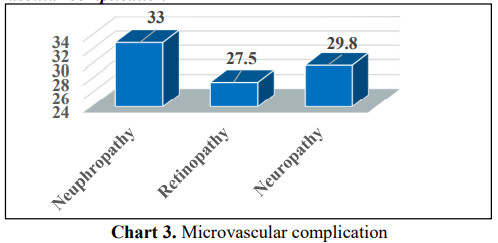
Microvascular complication includes nephropathy, retinopathy, and peripheral neuropathy.
In which peripheral nerve complication has a relatively close relationship with skin lesions in diabetic patients. Peripheral neuropathy is an important risk factor in the formation of cutaneous manifestations, especially atrophy, onychodystrophy.
The mechanism may be due to peripheral neuropathy causing dry skin (xerosis), cracked skin, reduced pain sensation, thereby leading to skin atrophy, onychodystrophy and some other injuries.
In our study on 109 diabetic patients with cutaneous manifestations, up to 29.8% of patients had peripheral nerve complication.
According to research by Duriye (2013) and Zahra (2019), the percentage respectively were 23.3% and 25.8% [3],[4]. Thus, our results are consistent with those of other authors around the world.
3.3. Cutaneous manifestations of diabetic patients and the relationship between common skin lesions and the pathological features
3.3.1. Cutaneous manifestations of diabetic patients
Cutaneous infection
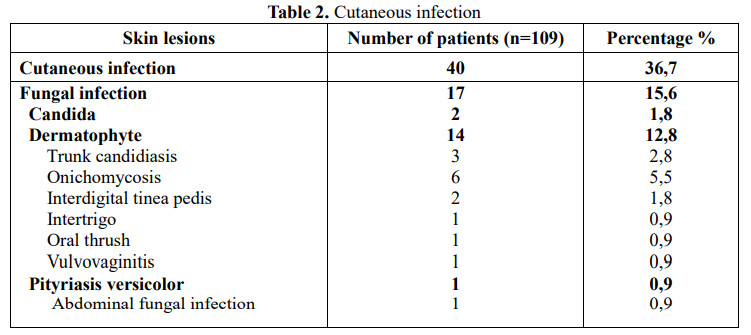
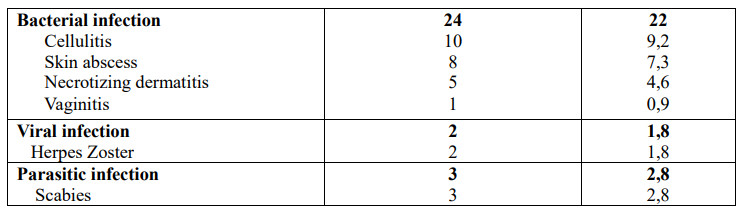
Poorly controlled diabetes patients have a high risk of systemic infection as well as skin infection. Many factors contribute to the mechanism of these lesions, in which high blood glucose level, changes in cellular immunity and vascular function play a prominent role.
40/109 patients in our study had cutaneous infection, equivalent to 36.7% and was one of the most common lesions.
Results from other studies have shown a high rate of skin infection in diabetic patients. According to a study by Duriye et al. (2013) on 750 diabetic patients, including 574 patients with skin lesions, skin infection (including bacterial infection, fungal infection and viral lesions) was the most common, accounting for 59.93% [3]. Another study conducted on 200 diabetic patients by Kumar et al. (2018) revealed the similar results with the rate of skin lesions of 55.5%, skin infection made up the highest rate (54 ,95%) [5].
Among skin infections, bacterial and fungal infection constituted the highest percentage, 22% and 15.6%, respectively.
The mechanism may be due to high blood glucose levels leading to a decline in leukocyte function creating favorable conditions for the growth of pathogenic bacteria and fungi.
Our results are consistent with some authors in the world. Nawaf et al. (2006) studied 106 diabetic patients, patients with skin infection accounted for 25.5% [6]. The study of Kumar et al. (2018) on 111 patients also demonstrated similar results to ours on bacterial infection (18.92%) [5].
Non-infectious cutaneous manifestations
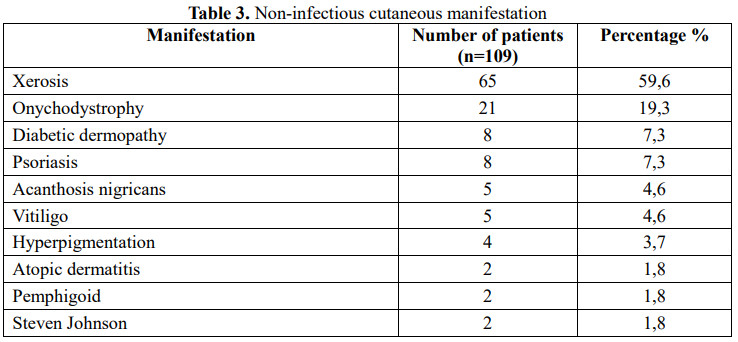
In our study, some common non-infectious cutaneous manifestations were xerosis, onychodystrophy, diabetic dermopathy and psoriasis, at the rate of 59.6%; 19.3%; 7.3% and 7.3%, respectively.
The lack of moisture in the stratum corneum and decreased activity of the sebaceous glands in diabetic patients lead to clinically observed xerosis. On the other hand, in diabetic patients, albeit xerosis may not appear, the renewal process of the stratum corneum has been damaged. In addition, nail thickening and excessive nail deformity are typical features of onychodystrophy and may indirectly lead to toe infection.
Wearing ill-fitting shoes can cause repeated injuries and worsen infection. In patients with diabetes, onychodystrophy is a consequence of peripheral hypoperfusion associated with diabetic neuropathy and can cause diabetic foot ulceration.
Proper nail care, wearing the right shoe size, and early attention to nail infection are all measures to limit the progression of lesions.
3.3.2. The relationship between some common cutaneous manifestations and features of diabetes mellitus
The relationship between some common cutaneous manifestations and disease duration
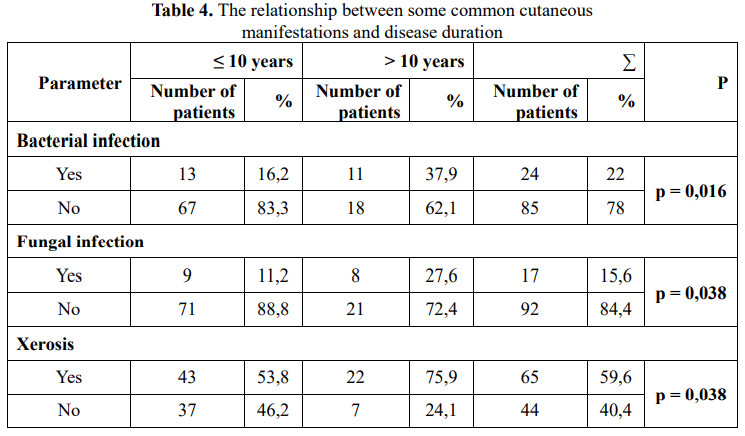
Our results indicated that bacterial infection, fungal infection and xerosis were correlated with the duration of the disease. Most of the studies on cutaneous manifestations and duration of diabetes have demonstrated a consistent result that there is a significant relationship between the two factors. The longer patients have diabetes, the more likely they are to have skin diseases. The cutaneous manifestations in diabetic patients are diverse in both morphology and quantity. Therefore, it is necessary for physicians to pay attention to early detection of these lesions and coordinate with dermatologists for timely diagnosis and treatment, avoiding progression to serious complications.
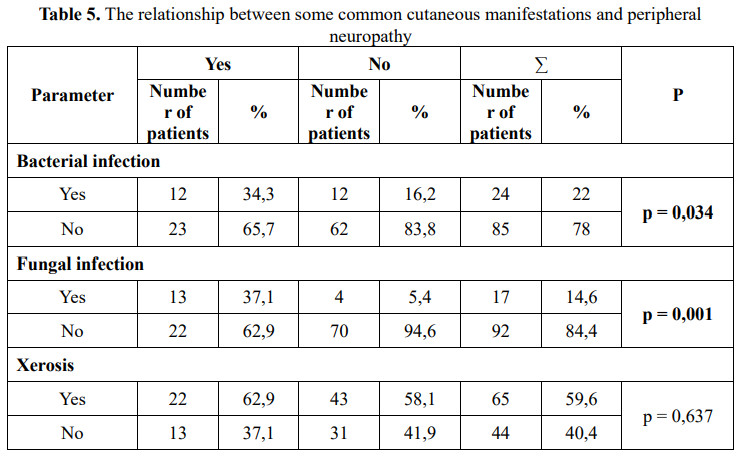
The relationship between some common cutaneous manifestations and peripheral neuropathy
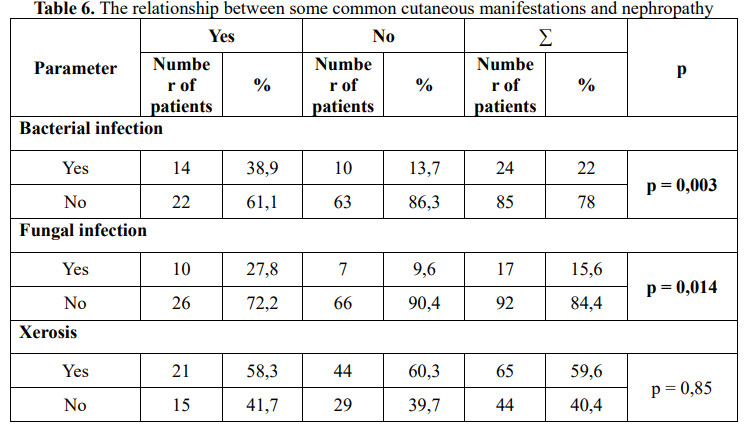
The relationship between some common cutaneous manifestations and nephropathy
The relationship between some common cutaneous manifestations and retinopathy
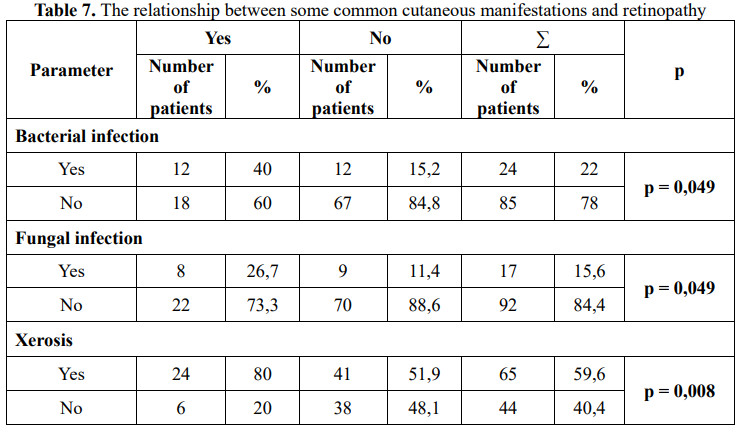
Investigating common cutaneous manifestations and microvascular complication, we found that the proportion of patients with bacterial infection and fungal infection was higher than that of patients with retinopathy, peripheral neuropathy and nephropathy compared with the group of those without complications, with statistically significant difference (p < 0.05).
In addition, the rate of xerosis was also significantly higher in the group of patients with retinal complication compared to that of those without this complication. However, there was no association among other lesions such as diabetic dermopathy, psoriasis, onychodystrophy.
The risk of systemic infection and skin infection in particular is higher in patients with high blood glucose level and changes in cellular immune function [7]. On the other hand, duration of diabetes and poor glycemic control are risk factors for microvascular complication.
This may explain the significant relation between bacterial and fungal infection and microvascular complication.
Our findings have some similarities with the results from study of Duriye et al. on 750 diabetic patients in which 594 patients had cutaneous manifestations.
In this study Duriye found a significant correlation between the proportion of cutaneous infection with renal complication and peripheral neuropathy, the percentage of fungal infection was also correlated with nephropathy and retinopathy complication [2].
In addition, Hosseini et al. (2006) studied the association between cutaneous manifestations and microvascular complication on 1135 patients with type 2 diabetes, the author observed that retinopathy and peripheral neuropathy occurred more frequently in patients with skin lesions [8].
On the other hand, further evaluation of the association between cutaneous manifestations and macrovascular complication such as cerebrovascular accident, coronary artery disease, peripheral artery disease should be investigated, we did not find the correlation through our study.
4. CONCLUSION
Common cutaneous manifestations in diabetic patients are bacterial infection, fungal infection, xerosis, onychodystrophy and diabetic dermopathy.
Most of them are associated with disease duration and microvascular complication of diabetes.
Therefore, physicians should be aware of these lesions for early detection and prompt treatment, contributing to improve the quality of life and comprehensive patient care, as well as limiting complications of chronic hyperglycemia.
REFERENCE
1. International Diabetes Federation. Diabetes complication. IDF Diabetes Atlas, t.E.B., Belgium: International Diabetes Federation. 2017, 82-95.
2. Demirseren DD, E.S., Akoglu G, et al. Relationship between skin diseases and extracutaneous complications of diabetesmellitus: clinical analysis of 750 patients. Am J Clin Dermatol 2014; 15:65 – 70.
3. Demirseren, D.D., Emre, S., Akoglu, G. et al. Relationship Between Skin Diseases and Extracutaneous Complications of Diabetes Mellitus: Clinical Analysis of 750 Patients. Am J Clin Dermatol. 2014; 15, 65–70.
4. Zahra A, Elham B, Roshanak H, et al. Prevalence Study of Dermatologic Manifestations among Diabetic Patients. Adv Prev Med. 2019; 2019: 5293193.
5. Kumar Satya Prakash, Ichchhit Bharat. Cutaneous manifestations in patients with diabetes mellitus in a tertiary care hospital at Bihar, India: An Observational Study. Journal of medical science and clinical reseach. 2018;07:717-724
6. Nawaf Al-Mutairi, Amr Zaki, Ashok Kumar Sharma, Mazen Al-Sheltawi. Cutaneous manifestations of diabetes mellitus. Study from Farwaniya hospital, Kuwait. Med Princ Pract. 2006;15(6):427- 30.
7. Levy L, Zeichner JA. Dermatologic manifestation of diabetes. J Diabetes. 2012;4:68–76.
8. Hosseini M, Ehsani AH, Farhad HP, et al. The Correlation between Skin Lesions, Microalbuminuria and other Microvascular Complications in Type 2 Diabetic Patients. Int J Nephrol Urol. 2010;2(4): 553-560.
 Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam
Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam Hội Nội Tiết – Đái Tháo Đường Miền Trung Việt Nam